Site Selection & Qualification Visits: Essential Guide for CRAs
Clinical trial success doesn’t begin with patient enrollment—it starts with precise site selection and qualification. These visits form the foundation of a trial’s execution, ensuring that only competent, compliant, and resource-equipped sites are brought onboard. For Clinical Research Associates (CRAs), mastering the intricacies of these visits is critical. A single oversight during qualification can result in recruitment delays, protocol violations, or regulatory scrutiny down the line. Sponsors don’t just expect thoroughness—they demand proactive risk mitigation.
This guide goes deep into what site selection and qualification visits teach aspiring and active CRAs. From regulatory-mandated assessments to red flag identification, we break down the questions that must be asked, documents that must be collected, and judgment calls that must be made. Whether you're new to clinical research or preparing for senior CRA roles, you’ll learn how certification programs like the Advanced Clinical Research Associate Certification (ACRAC) from CCRPS equip professionals with real-world, inspection-ready skills.
What Are Site Selection & Qualification Visits?
Purpose and Regulatory Mandates
Site selection and qualification visits are not administrative formalities—they are legally and operationally indispensable checkpoints mandated by global regulatory authorities. Agencies like the FDA, EMA, and MHRA require sponsors and CROs to verify that investigational sites have the infrastructure, staffing, and compliance systems necessary for trial execution. For sponsors, these visits are also a risk-assessment process aimed at preventing deviation-prone environments.
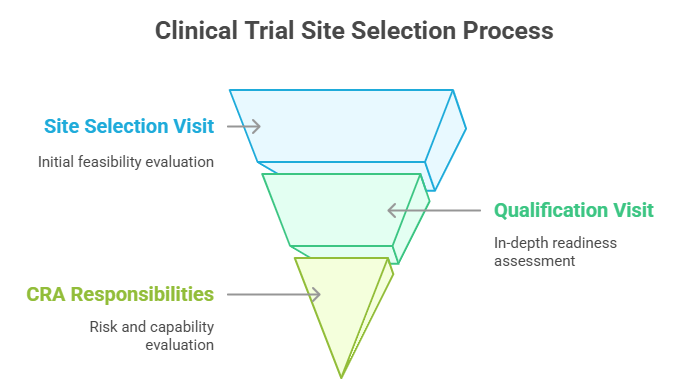
A site selection visit typically occurs early in the clinical development timeline—often before protocol finalization. It evaluates whether the site is even worth qualifying. The qualification visit, on the other hand, is conducted once preliminary interest is confirmed and assesses the site's readiness for activation, including ICH-GCP compliance, PI suitability, and logistical capacity. These visits ensure that enrollment targets are achievable and that data integrity will not be compromised.
Timing in the Trial Lifecycle
In the clinical trial lifecycle, site visits are strategically placed before contracting and site initiation. Site selection visits generally occur 6–12 months prior to First Patient In (FPI). During this phase, CRAs are responsible for preliminary vetting, assessing feasibility, and reporting initial findings. It is during these visits that the sponsor makes critical Go/No-Go decisions.
Qualification visits follow shortly after selection, especially for high-recruiting protocols or global trials. The visit includes a comprehensive walkthrough of SOPs, quality systems, and staff credentials, ensuring the site can handle regulatory inspections at any time. For CRAs, this is where observational skill, protocol knowledge, and regulatory literacy converge to assess whether the site can realistically meet trial demands without escalating risk exposure.
Key Criteria Used During Site Feasibility
PI Experience, Site Infrastructure, Recruitment Potential
When evaluating clinical trial sites, CRAs don’t just tick boxes—they strategically interrogate a site’s capacity, credibility, and consistency. The most critical element is the Principal Investigator (PI). Sponsors expect PIs to have prior GCP-compliant trial experience, documented inspection readiness, and a strong publication or regulatory history. A site may have high patient volume, but without a capable PI, it's a regulatory liability.
Next is site infrastructure. This includes the availability of temperature-monitored drug storage, private consultation rooms, secure data archiving systems, and 24/7 access to emergency equipment. A well-equipped site is more likely to comply with Good Clinical Practice (GCP) and avoid protocol deviations that can delay approvals or compromise data.
Another major factor is recruitment potential. Sites must demonstrate access to the target patient population within the trial’s inclusion/exclusion criteria. CRAs evaluate historical recruitment data, screen failure rates, and local standard-of-care overlaps. Sites that overpromise recruitment without data to back it up are flagged as high-risk. Conversely, those that present patient databases, pre-consent workflows, and EHR query systems show strong feasibility.
A seasoned CRA uses these three axes—PI, infrastructure, and recruitment—to determine if a site can be qualified for high-quality, low-risk execution.
Questions CRAs Must Ask During Visits
SOPs, Storage, Staffing, EDC Access
CRAs are not passive observers during site qualification—they are active interrogators of operational readiness. The strength of a qualification visit lies in the questions asked. One of the first areas of focus is Standard Operating Procedures (SOPs). CRAs must verify whether site SOPs align with ICH-GCP, especially regarding informed consent, AE/SAE reporting, and investigational product (IP) handling. Asking for documented SOP version control, training logs, and deviation reporting flowcharts reveals how mature a site’s compliance culture is.
Next is storage of investigational products and essential documents. CRAs should request a physical walkthrough of IP storage areas to confirm temperature monitoring, restricted access, and alarm systems. The same applies to document storage—GCP requires archiving to prevent tampering or unauthorized access. Questions here might include: “How are backups handled?” or “Who has document room access after hours?”
Then comes staffing. A frequent cause of mid-trial failure is understaffing or staff turnover. CRAs should ask: “What happens if your study coordinator resigns mid-trial?” and “How many trials are your team managing concurrently?” Sites must show redundancy plans and backup staff training protocols.
Finally, EDC (Electronic Data Capture) access and training must be confirmed. CRAs should ask whether coordinators have prior experience with the EDC system specified in the protocol. A delay in EDC onboarding often leads to late data entry, missed queries, and audit findings—all avoidable with the right questions.
| Component | Description | Purpose/Impact |
|---|---|---|
| SOPs | Verify alignment with ICH-GCP, request version control logs, consent and AE/SAE handling procedures | Assesses compliance maturity and procedural consistency |
| Storage | Inspect IP and document storage for temperature control, restricted access, and alarm systems | Ensures data integrity and drug accountability |
| Staffing | Ask about turnover plans, workload capacity, and backup personnel training | Evaluates operational stability and trial continuity |
| EDC Access | Confirm coordinator experience with the EDC system and training completion | Prevents data delays and minimizes audit risk |
Documents to Collect During the Qualification Visit
CVs, GCP Certificates, Protocol-Specific Logs
CRAs must exit every qualification visit with a clear paper trail that proves due diligence. That begins with signed and dated CVs for all key personnel—especially the PI, sub-investigators, and study coordinator. These CVs must demonstrate relevant therapeutic experience, recent clinical trial involvement, and current licensure. Any outdated CV raises flags during sponsor audits or regulatory inspections.
Next are Good Clinical Practice (GCP) certificates. Sponsors require documented proof that all site personnel handling patient data or investigational product have completed ICH-GCP training within the past 2–3 years. CRAs should verify authenticity, check completion dates, and document which training vendor was used (e.g., TransCelerate-recognized providers). Sites without current GCP certificates are often barred from activation.
CRAs must also collect protocol-specific logs that reflect the site’s preparedness. This includes delegation of authority logs, lab normal ranges, calibration certificates for study-critical equipment, and SOP sign-off sheets related to the protocol. These documents help confirm that the site understands the study-specific requirements and is preparing for immediate readiness upon activation.
It’s not just about gathering files—it’s about interpreting what they reveal. Missing documentation often points to poor coordination or lack of regulatory awareness, both of which are red flags for sponsors.
| Document Type | Description | Purpose/Impact |
|---|---|---|
| CVs of Key Personnel | Signed, dated CVs for PI, sub-investigators, and coordinator showing trial experience and licensure | Verifies qualifications and satisfies regulatory expectations |
| GCP Certificates | Proof of ICH-GCP training completed within the last 2–3 years; must be vendor-recognized | Confirms GCP compliance and eligibility for trial participation |
| Protocol-Specific Logs | Delegation logs, lab ranges, calibration certificates, and protocol-specific SOP acknowledgments | Demonstrates operational readiness and protocol awareness |
Site Selection Mistakes That Risk Trial Integrity
Overpromising Sites, Lack of PI Availability
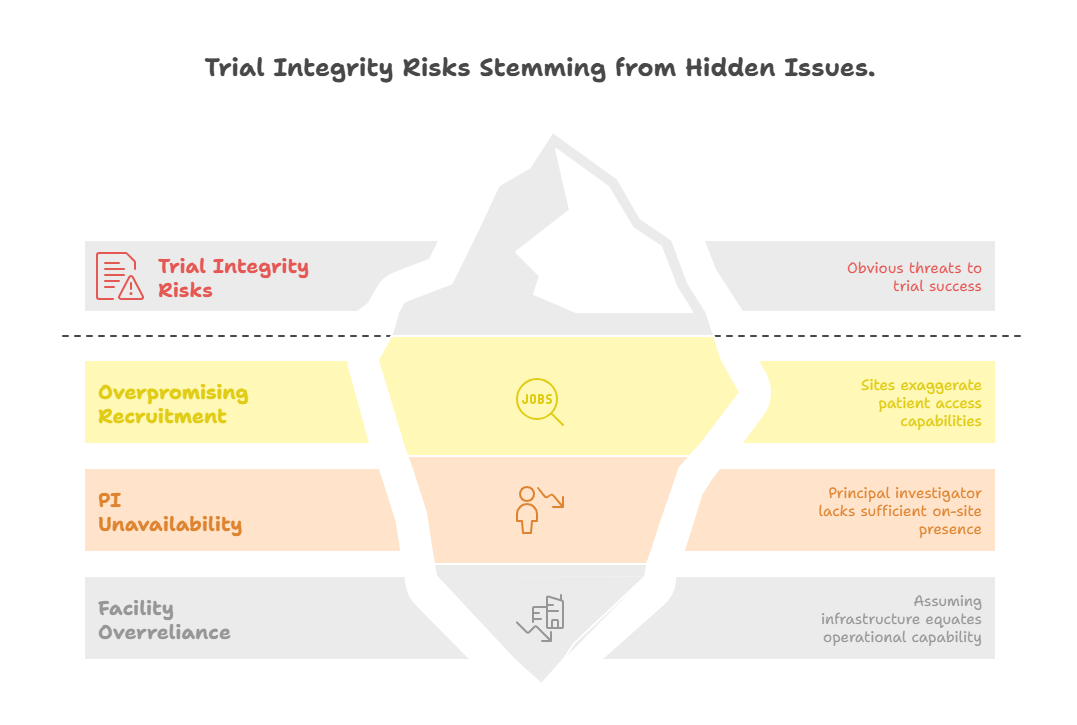
Even experienced CRAs can fall into traps during site selection—especially when pressed by sponsors to meet startup timelines. One of the most damaging mistakes is choosing sites that overpromise on recruitment. A PI may claim access to 1,000 eligible patients but provide no data to support it. When sites inflate recruitment potential to secure participation, trials face delayed enrollment, budget overruns, and protocol amendments to widen inclusion criteria—all of which erode trial validity.
Another common failure point is not verifying PI availability. The PI may be involved in multiple concurrent studies, administrative roles, or have limited clinical hours. CRAs must quantify PI bandwidth: How many active trials is the PI leading? How often will they be on-site? Without hands-on oversight, key responsibilities like adverse event assessment, source document verification, and protocol adherence are delegated—leading to quality dilution and audit exposure.
CRAs must also avoid relying on “impressive facilities” as a proxy for competence. A hospital with cutting-edge imaging or electronic systems may still lack trial coordination maturity. What matters is whether the site has demonstrated operational follow-through in real-world trials. That’s why seasoned CRAs document every assumption and probe beyond surface-level metrics.
Sponsor Expectations from Qualification Reports
Red Flags and Final Recommendations
The qualification report isn’t a summary—it’s a decision-making tool. Sponsors rely on this document to evaluate whether a site is not just compliant, but strategically valuable to the study. They expect CRAs to deliver more than checklists—they expect clear, evidence-based recommendations backed by investigative rigor. Every report should detail observed strengths, logistical risks, and unresolved concerns with actionable insights.
A major sponsor priority is the identification of red flags. These include inconsistent responses during interviews, poor documentation hygiene, outdated SOPs, and overly reliant staff hierarchies. For example, if only one coordinator handles all trials and can’t articulate protocol nuances, the site is at risk of bottlenecks. Sponsors expect CRAs to spot such fragilities and not sugarcoat them. Vague or overly optimistic reports are considered compliance liabilities.
CRAs are also expected to justify their Go or No-Go recommendations. “Recommended with conditions” must be backed by timelines and corrective actions—such as “PI to complete GCP training before SIV” or “Backup coordinator to be formally delegated.” The best CRAs are not neutral—they take a stand, backed by protocol needs, patient safety priorities, and regulatory readiness. A well-written qualification report can preempt protocol deviations months before they occur.
How Our ACRAC Course Trains You for Site Visits
The Advanced Clinical Research Associate Certification (ACRAC) offered by CCRPS doesn’t just teach theory—it prepares CRAs for real-world qualification visits with precision, foresight, and sponsor-aligned rigor. Our curriculum goes far beyond ICH-GCP basics to deliver actionable training in feasibility analysis, document auditing, protocol-specific questioning, and investigational product handling compliance.
Trainees engage with interactive simulations that mirror actual qualification visits, where they must identify red flags, interview site staff, and draft recommendation reports that would pass sponsor review. They’re trained to recognize subtle compliance gaps—such as undocumented training, data security vulnerabilities, or PI delegation issues—that can derail trials later.
Through expert-led modules, learners also gain deep familiarity with site infrastructure checklists, regulatory inspection readiness, and stakeholder communication protocols. Whether you're qualifying a site for a rare disease trial or a high-volume oncology study, the ACRAC course ensures you’re equipped to ask the right questions, collect the right documents, and make the right calls—every time.
Frequently Asked Questions
-
A site qualification visit evaluates whether a clinical trial site meets the operational, regulatory, and logistical criteria necessary to run a specific study. It’s not just about ticking compliance boxes—it's about assessing the site's real-world readiness to recruit, retain, and report. CRAs investigate everything from PI qualifications and infrastructure to SOP adherence and staff bandwidth. These visits help sponsors avoid costly mistakes like non-enrolling sites, regulatory violations, or data quality issues. By validating each site before activation, qualification visits reduce trial delays and ensure that only high-performance locations make it into the final site list. Sponsors rely heavily on CRA reports from these visits to guide Go/No-Go decisions.
-
CRAs must gather essential documents that prove the site’s regulatory compliance and operational capability. These include signed CVs for all investigators, GCP training certificates (within the last 2–3 years), protocol-specific delegation logs, and equipment calibration records. In addition, they collect SOP version logs, lab normal ranges, and facility licenses. These records serve two critical purposes: they allow sponsors to verify site credentials before trial activation and form part of the site master file for audit readiness. Missing or outdated documents during qualification visits can delay startup and flag the site as high-risk. CRAs must verify authenticity and completeness on-site.
-
Site qualification visits should be scheduled well before the site initiation visit (SIV) and ideally 4–6 months prior to First Patient In (FPI). In global or multi-site studies, this window may extend to 6–12 months to accommodate travel logistics and regulatory review timelines. These visits must happen after the feasibility assessment but before contracts and study supplies are deployed. The timing ensures that sponsors can act on CRA recommendations—whether approving, rejecting, or conditionally accepting a site—without jeopardizing overall trial timelines. Delaying qualification visits risks onboarding non-compliant sites or compressing timelines so tightly that protocol deviations become inevitable.
-
CRAs must probe beyond surface-level confidence. They should ask: “Do you have documented SOPs for informed consent and AE reporting?” “What is your backup plan if the coordinator is unavailable?” and “Have you used this EDC system before?” These questions test regulatory literacy, staffing stability, and tech readiness. CRAs should also inquire about data security measures, storage conditions for investigational product, and any inspection history. Vague or overly optimistic answers are red flags. A skilled CRA adapts the question set based on protocol needs, ensuring that every visit reveals operational strengths and latent weaknesses that could compromise study success.
-
Sponsors must treat CRA qualification reports as a strategic risk dossier. Major red flags include outdated GCP training, a PI with limited availability, lack of SOP adherence, inconsistent interview responses, or inadequate infrastructure for IP storage. Reports that downplay or omit such issues often backfire during trial execution. Sponsors should also be wary of sites that overpromise on recruitment without patient database evidence. Incomplete or templated CRA reports are also problematic—they suggest insufficient site interrogation. A sponsor-ready report will not only flag issues but recommend corrective actions and offer a confident, evidence-backed Go/No-Go recommendation.
-
The Advanced Clinical Research Associate Certification (ACRAC) trains CRAs in real-world site qualification techniques through simulation-based modules, expert-led walkthroughs, and documentation reviews. Trainees learn to ask the right feasibility questions, identify subtle compliance gaps, audit regulatory documents, and produce inspection-grade reports. The course places special focus on sponsor expectations, protocol-specific analysis, and regulatory readiness. CRAs gain fluency in identifying red flags, drafting actionable recommendations, and ensuring that each qualified site contributes to risk-mitigated trial outcomes. Graduates walk away with the confidence to lead qualification visits independently and meet the operational expectations of global sponsors and CROs.
-
If a site fails a qualification visit, it’s typically disqualified from participating in the trial unless critical issues are addressed within a defined timeframe. CRAs document the deficiencies—such as expired licenses, lack of GCP training, or infrastructural gaps—in their qualification report. Sponsors may issue a conditional approval pending correction, but only if the site shows strong potential. Sites that show systemic issues like high staff turnover or non-functional SOP systems are generally excluded to protect data integrity. Qualification visit failures are not just about compliance—they're about protecting trial timelines, participant safety, and regulatory success down the line.
Our Verdict
Site qualification is where trials succeed—or silently fail. For CRAs, these visits are not routine—they are mission-critical checkpoints that determine whether a trial runs on time, on budget, and in full compliance. Sponsors depend on evidence-driven reports, not vague assurances, to select high-performing sites. And sites depend on skilled CRAs to guide them through readiness with precision.
The Advanced Clinical Research Associate Certification (ACRAC) from CCRPS gives CRAs the technical fluency, regulatory depth, and real-world judgment to excel in this role. Whether you’re assessing SOP quality, auditing storage infrastructure, or identifying hidden risks, this certification ensures you’re not just conducting visits—you’re protecting trial integrity at its core.