Triage Definition: The Ultimate Guide to Understanding The Meaning of Triage (Definition & Practices) - 2025 Edition
Triage is a term that resonates across multiple disciplines, from healthcare and emergency management to business strategy and IT systems. But what exactly does it mean, and why is it so important in critical decision-making? This guide unpacks the definition of triage, highlights its applications, and explores its relevance through engaging examples and actionable insights.
What Is Triage?
At its simplest, triage is the practice of allocating limited resources or assigning workload to various tasks, or people according to the level of requirement or need. The term triage is originated from the French word ‘trier’ which means ‘to sort’ and at its purest form, triage is the decision making tool used especially during resource constrained or critical situations.
The Three Pillars of Triage
Prioritization: Deciding which cases or tasks are the most urgent.
Resource Allocation: Determining how to efficiently use limited tools, personnel, or time.
Continuous Evaluation: Reassessing priorities as conditions evolve.
Triage ensures that the most pressing needs are addressed first, ultimately limiting risk and achieving optimal outcomes.
The Three-Category Triage System
Triage is a tool that healthcare professionals primarily use to prioritize patients in emergency care or disaster settings. Here is a breakdown of the commonly employed three-category triage system:
Immediate (Red): Critical cases requiring life-saving interventions (e.g., cardiac arrest).
Delayed (Yellow): Serious but not life-threatening; treatment can be postponed slightly (e.g., fractures).
Minor (Green): Non-urgent cases requiring basic treatment or observation (e.g., minor cuts).
Actionable Tips for Triage Application
The effectiveness of any triage system depends on the correct balance of urgency, resource capability, and outcomes. To optimize the triage process, follow these actionable steps.
Steps for Effective Triage
Establish Clear Criteria: Define what qualifies as high, moderate, and low priority. Use objective measures to prevent bias.
Integrate Technology: Tools like resource management software or automated alert systems improve efficiency and trackability.
Train Your Team: Conduct simulations to prepare staff for high-pressure decision-making scenarios.
Why Clinical Research?
Clinical research is a vital role in advancing medicine and it needs exceptional organizational, analytical and problem solving skills. The transition into clinical research provides a chance to blend competitive salaries with a meaningful contribution to healthcare innovation.
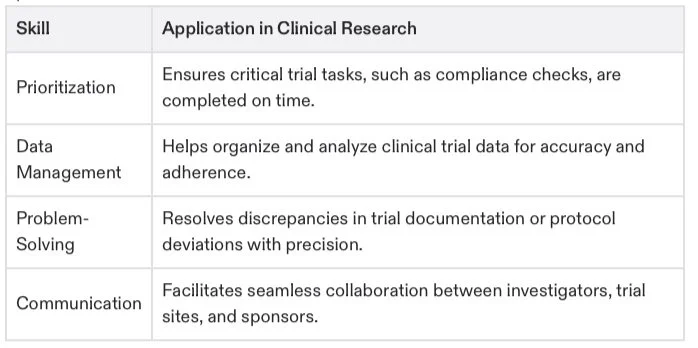
Key Transferable Skills
You might not realize it, but common triage-related skills are highly valuable for clinical research roles like Clinical Research Associates (CRA), Data Managers, or Regulatory Specialists.
Actionable Steps to Transition
Gain Certification: Get certified through programs like CCRPS to gain credibility and foundational knowledge. Certification not only provides the necessary competencies but also ensures regulatory readiness for clinical trials.
Highlight Your Experience: On your resume, emphasize how skills like prioritization and resource allocation from your current role are directly applicable to trial monitoring and patient safety.
Network Effectively: Join clinical research communities or forums to connect with professionals, access opportunities, and learn the industry's nuances.
Assess Your Readiness: Take the CCRPS Certification Quiz to determine how ready you are to step into clinical research and identify areas of improvement.
Take Free CCRPS Career Quiz Today
The Meaning of Triage: Triage in Pharmacovigilance and Clinical Research
Clinical research is a dynamic field where new findings shape future healthcare innovations. While “triage” might recall an emergency room setting, it also plays a critical role in research management. Triage in clinical research is essential for prioritizing the enrollment of participants, optimizing resources, and driving impactful results. This guide unpacks the meaning of triage, its applications in clinical trials, and actionable strategies to ensure impactful collaboration and outcomes.
For professionals looking to expand their clinical research expertise, this guide also provides direct links to certifications and training programs to propel your career forward on platforms like CCRPS.
Key Goals in Clinical Research Triage
Efficient Participant Selection: Identifying individuals who meet specific eligibility criteria ensures resources aren't wasted, and trials proceed smoothly. To improve your expertise in this area, check out the Clinical Research Coordinator Course.
Maximizing Trial Success: Prioritizing optimal matches between participants and trial objectives improves meaningful outcomes. Learn more about best practices for maintaining trial safety in the Pharmacovigilance Certification.
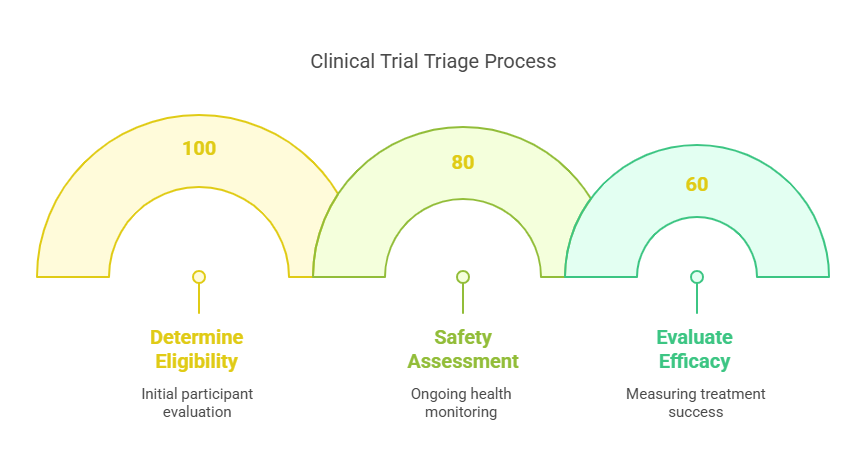
The Steps of Triage in Clinical Trials
Triage in clinical trials is a structured process that ensures the efficient use of resources, while keeping patient safety and trial success at the forefront. Here is a step-by-step look at how triage functions in this context:
1. Determine Eligibility
The first and most critical step in clinical trial triage is establishing eligibility. Researchers evaluate participants based on specific criteria such as age, medical history, condition severity, and treatment status. These factors ensure that only individuals who align with the trial’s objectives are enrolled.
Why It Matters: Screening participants saves time and prevents resources from being spent on ineligible cases. It helps trials stay focused and efficient.
Tools & Training: Many trials now incorporate Electronic Health Records (EHRs) to verify eligibility. Explore more about trial coordination with the Clinical Research Coordinator Course.
2. Safety Assessment
The next step involves continuous monitoring of trial participants to safeguard their health. Researchers look for potential adverse events (AEs) or any sign of harm stemming from the investigational drug or treatment.
Action Plan:
Serious adverse events result in immediate suspension of treatment for the affected participant.
Medical care is provided promptly to address any observed risks.
Reliable safety assessment not only protects participants but also prevents regulatory issues that could halt the trial. Build expertise in safety monitoring through the Medical Monitor Certification.
3. Evaluate Efficacy
Finally, researchers assess how well the drug or treatment worked compared to placebo or standard care. This step determines whether the treatment has achieved its intended goals with minimal side effects.
Outcome: If the data points to safety and success, the treatment may move one step closer to regulatory approval.
4. Building Efficiency with Triage
Triage in clinical trials ensures that each phase—eligibility, safety, and efficacy—is properly executed. For those aspiring to play a pivotal role in carrying out these steps, the ICH-GCP Certification provides valuable insights into global clinical trial standards.
How Triage Prioritizes Patients in Clinical Research
Prioritizing patients in clinical research is both an art and a science. By sorting participants based on their level of need and suitability for the study, triage allows researchers to focus on the individuals most likely to benefit from treatment—and, in turn, contribute to meaningful outcomes. Here’s what that process looks like in detail:
Factors That Influence Triage Decisions
Severity of Illness: Patients with life-threatening or advanced conditions often get priority in trials designed for urgent interventions.
Resource Availability: Trials have limited resources, from study slots to medical staff, requiring careful prioritization to maximize efficiency.
Study Type: Some trials are intentionally designed to recruit only the most severe or uncommon cases.
Existing Patient Data: Patients with prior records of similar treatment can be excluded to avoid redundancy.
Key Insight: Those patients deemed high-risk or ineligible are excluded not to deny them care, but to ensure their safety, as some treatments could amplify risks.
Benefits of Triage in Clinical Trials
Triage brings substantial benefits for both researchers and patients, fostering an environment of streamlined operation and improved outcomes.
For Researchers
Efficient Resource Management: Triage ensures that time, funding, and personnel are used where they will make the greatest impact.
Faster Data Collection: By enrolling the most eligible patients, researchers gather higher quality data in a shorter time span.
Enhanced Collaboration: Clinical staff, data scientists, and regulators work seamlessly when decision-making is guided by triage principles.
Learn More: Build your collaborative skills with the CRA Course.
For Patients
Priority Access to Treatment: Patients with critical needs gain timely inclusion in trials offering life-changing therapies.
Personalized Care: Researchers ensure each patient receives the care that aligns best with their condition.
Improved Health Outcomes: Triage helps patients participate in well-structured trials with strong safety protocols.
Tips for Effective Triage in Pharmacovigilance
Triage also plays a critical role in post-market surveillance and pharmacovigilance. Here are actionable tips for clinical research professionals responsible for monitoring drug safety.
Categorize Potential Risks: Use a risk matrix to prioritize adverse drug events (ADEs) by severity, likelihood, and population impact.
Utilize Alert Systems: Automate and centralize reporting systems for ADEs to identify safety trends faster. Access tools with the Pharmacovigilance Certification.
Continual Training: Equip all team members with up-to-date training on drug safety monitoring. Explore options through ICH-GCP Certification.
Beyond Proficiency—The Importance of Collaboration
Knowing the nuances of triage is only half the equation. To truly excel, professionals must master collaboration across clinical teams. From physicians and nurses to data managers, ensuring consistent communication and shared understanding is critical for seamless trial execution.
Recommended Certification
Enhance collaboration skills by exploring the Clinical Research Associate (CRA) Course.
Key Certifications to Accelerate Your Growth:
Clinical Trials Assistant Training: Ideal for support roles in trial execution.
ICH-GCP Certification: Gain comprehensive knowledge of international clinical trial guidelines.
Advanced Principal Investigator Physician Certification: Tailored for medical professionals aspiring to lead trials.
By mastering the art of clinical triage, you'll help shape the future of medicine—one trial at a time. Begin your transformational career today by exploring all the available programs and quizzes at app.ccrps.org.
Frequently Asked Questions (FAQs)
-
The primary goal of triage is to prioritize patients, tasks, or resources effectively to ensure that those most in need of immediate attention or intervention receive it first, maximizing the overall outcome in resource-limited settings.
-
In emergency healthcare, triage involves assessing patients' conditions using specific criteria to categorize them into urgency levels—typically immediate, delayed, or minor. This categorization helps medical personnel focus on treating the most critical cases first to improve survival rates and resource allocation.
-
Yes, triage can be applied in business settings to prioritize tasks or projects based on their importance and urgency. This helps organizations allocate resources efficiently and address the most critical issues that could impact business operations or profitability.
-
Key skills include strong analytical abilities, decision-making under pressure, knowledge of clinical protocols, and the ability to assess and prioritize research activities or patient needs quickly and accurately.
-
Relevant certifications might include Clinical Research Coordinator (CRC), Certified Clinical Research Associate (CRA), and Good Clinical Practice (GCP). These certifications ensure that professionals are knowledgeable about the latest guidelines and effective practices in clinical trials.
-
Triage improves outcomes by ensuring that resources such as time, personnel, and funding are concentrated where they can have the most impact, thus enhancing the efficiency of the trial and the quality of the data collected.
-
Technology plays a critical role in modern triage systems by providing tools such as electronic health records (EHRs), automated alert systems, and digital assessment tools that streamline the process of evaluating and prioritizing patients or tasks.
-
In IT systems management, triage is used to prioritize issues based on their impact on business operations. Critical system issues that could lead to significant downtime or data loss are addressed immediately, while less urgent issues are scheduled for later resolution.