The Beginner’s Guide to Remote Patient Monitoring
Remote Patient Monitoring (RPM) is revolutionizing healthcare delivery by enabling continuous patient care beyond traditional clinical settings. With the integration of digital technology, RPM allows for real-time health data collection and analysis, facilitating proactive medical interventions. As we navigate through 2025, understanding RPM's components, benefits, limitations, and emerging trends is crucial for both healthcare providers and patients.
What is Remote Patient Monitoring?
Remote Patient Monitoring (RPM) involves the use of digital technologies to collect health data from individuals in one location and electronically transmit it to healthcare providers in a different location for assessment and recommendations. This approach is particularly beneficial for managing chronic conditions such as hypertension, diabetes, and heart disease. By enabling continuous monitoring, RPM supports timely medical interventions and personalized care plans.
Related Blog: What Is Medical Monitoring and Why Does It Matter?
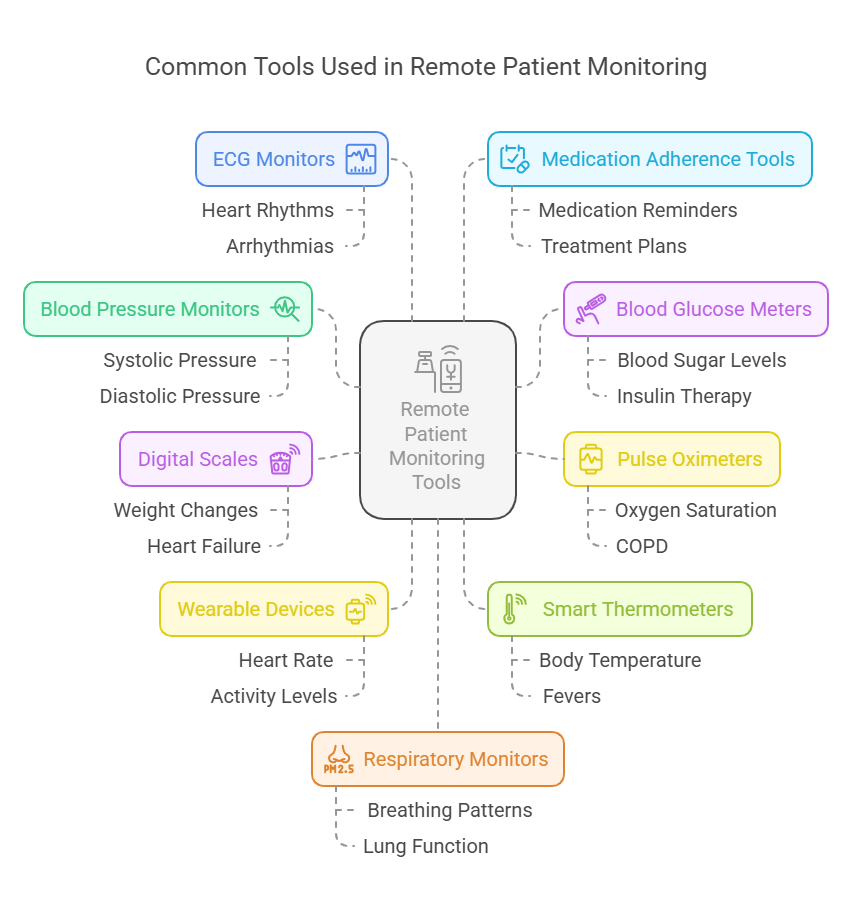
Common Tools Used in RPM
RPM utilizes a variety of devices to monitor different health parameters. These tools are designed to be user-friendly and integrate seamlessly with healthcare systems.
Blood Pressure Monitors: These devices measure systolic and diastolic pressure, transmitting data to healthcare providers for hypertension management.
Blood Glucose Meters: Essential for diabetic patients, these meters track blood sugar levels, aiding in insulin therapy adjustments.
Pulse Oximeters: Used to measure oxygen saturation levels, crucial for patients with respiratory conditions like COPD.
Digital Scales: Monitor weight fluctuations, important for patients with heart failure or obesity-related issues.
Wearable Devices: Smartwatches and fitness trackers monitor heart rate, activity levels, and sleep patterns, providing comprehensive health insights.
Smart Thermometers: Track body temperature to detect fevers, aiding in early infection detection.
ECG Monitors: Record heart rhythms, assisting in the detection of arrhythmias and other cardiac anomalies.
Medication Adherence Tools: Remind patients to take medications on time, ensuring compliance with treatment plans.
Respiratory Monitors: Measure breathing patterns and lung function, vital for asthma and COPD management.
Telehealth Platforms: Facilitate virtual consultations, allowing for real-time communication between patients and providers.
Related Blog: Top 10 Everyday Devices Use Medical Monitoring
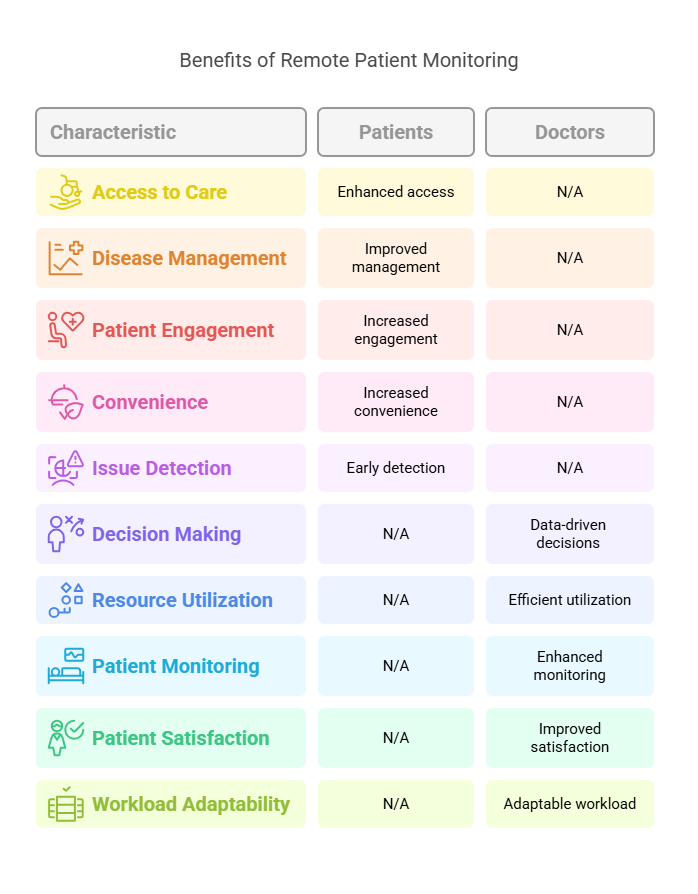
Benefits to Patients and Doctors
RPM offers numerous advantages that enhance healthcare delivery and patient outcomes.
For Patients:
Enhanced Access to Care: Patients in remote or underserved areas can receive quality care without traveling long distances.
Improved Disease Management: Continuous monitoring allows for timely adjustments to treatment plans, reducing complications.
Increased Engagement: Patients become active participants in their health, leading to better adherence to treatment regimens.
Convenience and Comfort: Monitoring health from home reduces the need for frequent clinic visits, saving time and resources.
Early Detection of Issues: Real-time data can alert healthcare providers to potential problems before they escalate.
For Doctors:
Data-Driven Decisions: Access to continuous data enables more informed clinical decisions and personalized care.
Efficient Resource Utilization: RPM can reduce hospital readmissions and emergency visits, optimizing healthcare resources.
Enhanced Patient Monitoring: Providers can keep track of patients' health status between visits, ensuring continuity of care.
Improved Patient Satisfaction: Timely interventions and personalized care plans contribute to higher patient satisfaction rates.
Adaptability to Workload: RPM allows for better management of patient loads, especially during times of increased demand.
Limitations and Concerns
Despite its benefits, RPM presents certain challenges that need to be addressed for optimal implementation.
Data Privacy and Security: Ensuring the confidentiality and security of patient data is paramount, requiring robust cybersecurity measures.
Technology Accessibility: Not all patients have access to the necessary devices or internet connectivity, leading to disparities in care.
User Proficiency: Some patients may struggle with using digital devices, necessitating additional support and education.
Integration with Healthcare Systems: Seamless integration of RPM data into existing electronic health records is essential for cohesive care.
Regulatory Compliance: Adhering to healthcare regulations and obtaining necessary approvals can be complex and time-consuming.
Lesser-Known Facts About RPM in 2025
AI Integration: Artificial intelligence is increasingly being used to analyze RPM data, predicting health trends and potential issues. (Source)
Virtual Hospitals: Institutions like Seha Virtual Hospital in Saudi Arabia are providing comprehensive care remotely, showcasing the potential of RPM. (Source)
Mental Health Monitoring: RPM tools are being adapted to monitor mental health indicators, aiding in early intervention strategies. (Source)
Chronic Disease Management: RPM is proving effective in managing chronic conditions, reducing hospital admissions and improving quality of life.
Elderly Care: RPM is enhancing care for the elderly, allowing for independence while ensuring health monitoring.
Postoperative Recovery: Patients recovering from surgery are benefiting from RPM through continuous monitoring and timely interventions.
Global Adoption: Countries worldwide are adopting RPM to address healthcare access challenges, especially in rural areas.
Environmental Impact: By reducing the need for travel, RPM contributes to lower carbon emissions, supporting environmental sustainability.
Insurance Incentives: Some insurance providers are offering incentives for patients who participate in RPM programs, recognizing its cost-saving potential.
Explore Courses for Clinical Research Career
Courses Available:
Conclusion
In conclusion, Remote Patient Monitoring (RPM) is shaping the future of healthcare by making it more accessible, efficient, and patient-centered. While it offers significant benefits like improved chronic disease management and reduced hospital visits, it also comes with challenges like data privacy and technology access. As RPM continues to evolve in 2025, it holds immense promise for transforming patient care when implemented thoughtfully. At CCRPS, we remain committed to supporting healthcare professionals with the training and tools needed to thrive in this digital health landscape.
Frequently Asked Questions (FAQs)
-
RPM is widely used to manage chronic conditions like hypertension, diabetes, heart failure, COPD, and obesity. It’s also increasingly being used for post-operative care, mental health monitoring, and maternal health tracking in 2025.
-
Yes. As of 2025, most insurance providers, including Medicare in the U.S., cover RPM services for eligible patients. However, coverage details can vary by provider and state, so it's best to consult your specific insurance plan.
-
Most FDA-approved RPM devices in 2025 are highly accurate and safe for home use. Devices such as blood pressure monitors, pulse oximeters, and continuous glucose monitors are designed for ease of use and data security.
-
Privacy concerns include the secure transmission and storage of health data. In 2025, healthcare providers must comply with updated HIPAA guidelines and use encrypted platforms to ensure patient data is protected.
-
RPM complements but does not replace in-person care. It helps reduce the frequency of visits by providing continuous data to healthcare providers, but physical exams and certain diagnostics still require in-office appointments.