Clinical Trial Medical Oversight: Essential Guide for Medical Monitors
Clinical trial medical oversight is the backbone of safe, compliant, and scientifically valid research. At the center of this oversight is the Medical Monitor—a licensed physician or domain expert responsible for safeguarding participant safety, ensuring protocol adherence, and interpreting critical data in real time. In 2025, as trials become more decentralized and globalized, medical oversight is no longer optional—it is a regulatory and ethical mandate.
This guide is designed for professionals stepping into, or advancing within, the oversight role. Whether you’re a clinical research physician, transitioning CRA, or part of a sponsor or CRO team, you’ll gain a granular understanding of medical monitor responsibilities, tools, regulatory intersections, and real-world execution. With adaptive trial designs, risk-based monitoring frameworks, and regulatory tightening across FDA, EMA, and MHRA, the medical monitor’s role has expanded beyond reactive review into proactive risk detection and cross-functional collaboration.
Role of Medical Monitors in Clinical Trials
Key Functions: Protocol Safety, Data Review, & Compliance
Medical Monitors are the primary medical authority during a clinical trial, acting as the first line of defense for participant safety and protocol integrity. Their core function is to evaluate clinical data in real-time, ensuring adverse events, efficacy trends, and deviation patterns are addressed without delay. While Principal Investigators (PIs) focus on site-level care, the monitor oversees the trial-wide medical narrative—from patient eligibility to emerging signal trends across sites.
This includes reviewing patient data for protocol compliance, validating endpoints, and identifying inconsistencies that could compromise trial results or trigger regulatory action. The monitor often flags issues such as improper dose modifications, unreported SAEs, or delayed lab result assessments. Their work ensures not just medical safety, but also audit readiness.
In 2025, medical monitors are expected to use AI-enhanced dashboards and real-time analytics, which drastically reduce review cycles while increasing accountability. With the shift to decentralized trials and remote source data verification, monitors now have broader visibility and less tolerance for data ambiguity.
Comparing Medical Monitors vs Principal Investigators
Although both roles are medical in nature, their scopes differ significantly. Principal Investigators manage on-site patient care, ensuring patients are treated ethically and in line with the protocol. Medical Monitors, on the other hand, operate at the trial-wide strategic level, interpreting aggregated data across all geographies.
PIs focus on recruitment, treatment delivery, and real-time assessments. In contrast, monitors are responsible for identifying cross-site trends, inconsistencies in AE reporting, and protocol drift. This distinction is critical when risk mitigation decisions must be made.
Unlike PIs, Medical Monitors frequently engage in protocol amendments, safety narrative reviews, and interactions with sponsors and Data Monitoring Committees (DMCs). Their role has expanded to include support for labeling discussions and regulatory responses, especially in pivotal Phase III studies.
Day-to-Day Activities of Medical Oversight
Medical oversight isn’t static—it evolves daily based on trial data flow. Below are the core recurring tasks:
Review cycles
Monitors participate in weekly or bi-weekly data review cycles, often involving cross-functional teams including biostatisticians, pharmacovigilance leads, and project managers. They assess patient narratives, lab trends, ECG anomalies, and any flagged case report forms (CRFs) that show deviations from expected safety profiles.
The goal of each cycle is to pre-emptively detect safety trends or compliance risks before regulators do. This includes preparing medical queries, follow-up actions, and interim medical safety reports that go to sponsors and ethics boards.
Documentation and deviation handling
Medical Monitors are responsible for preparing Medical Review Plans (MRPs) that define review frequency, thresholds for escalation, and protocol-sensitive parameters. When deviations occur—such as dosing outside of protocol or repeated late AE reporting—monitors document the issue, assign it a risk tier, and collaborate with the sponsor or site team on Corrective and Preventive Actions (CAPAs).
Proper documentation is key. Every escalation or deviation response must be logged with justification, medical rationale, and proposed resolution path. This process ensures transparency and shields both sponsors and investigators during audits or inspections.
Managing Safety Signals and Adverse Events
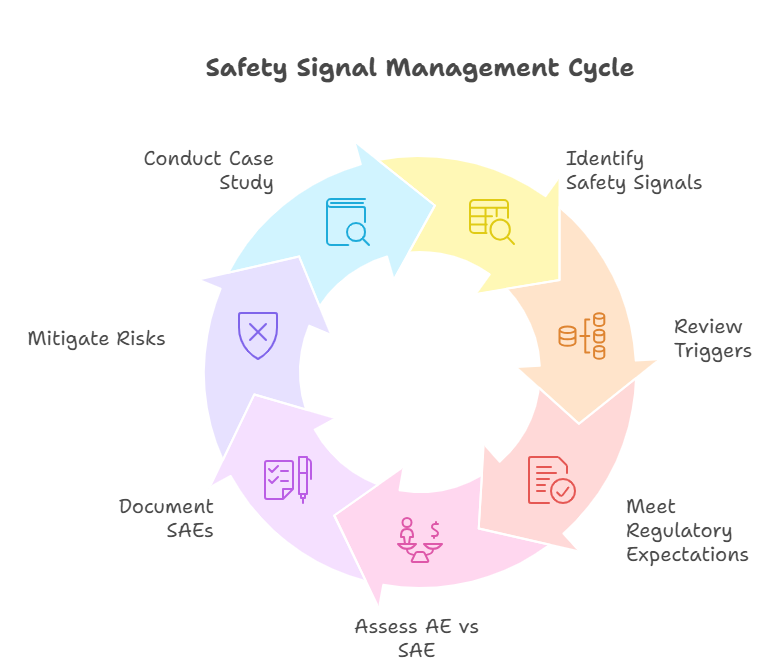
Identifying Safety Signals in Real-Time
In modern trials, the ability to identify emerging safety signals quickly can determine a study’s continuation—or its suspension. Medical Monitors track these signals across data streams such as electronic CRFs, lab reports, imaging results, and patient-reported outcomes. A safety signal doesn’t require statistical proof—it’s a clinically significant pattern that suggests a potential risk.
Common signals include clusters of elevated liver enzymes, consistent ECG abnormalities, or a higher-than-expected AE incidence in a treatment arm. AI tools may flag these early, but it’s the monitor’s clinical judgment that confirms whether escalation is warranted.
In 2025, global expectations from EMA, FDA, and MHRA mandate that safety signal detection must be continuous—not periodic. Therefore, monitors are expected to review new data at least weekly, if not more frequently during high-risk phases or dose escalations.
Adverse Event (AE) vs Serious AE (SAE): Key Differences
All AEs must be recorded, but not all are critical. Medical Monitors assess each event based on impact, severity, and expectedness. An Adverse Event might include nausea or mild headache, while a Serious Adverse Event (SAE) involves death, hospitalization, or persistent disability.
Monitors verify SAE documentation to ensure causality assessment, timelines, and seriousness criteria align with ICH-E2A guidelines. Failure to differentiate or escalate SAEs promptly is a leading cause of inspection findings and trial delays.
Moreover, determining “relatedness” is a nuanced task—requiring the monitor to evaluate co-medications, disease progression, and previous data. This judgment directly influences regulatory reports, interim safety updates, and protocol modifications.
Role in Medical Risk Mitigation Committees
Medical Monitors are often embedded in Safety Management Teams (SMTs) or Risk Mitigation Committees, where they contribute to strategic decisions like dose holds, trial pauses, or DMC advisories. These decisions are made using both statistical inputs and clinical reasoning.
The monitor may recommend changing inclusion criteria, halting a specific cohort, or adjusting monitoring intensity. Their input must be rooted in defensible data and backed by regulatory-aligned justification, as it will likely be audited during marketing application reviews.
Case Study: SAE escalation in Phase III oncology trial
In a global Phase III lung cancer study, Medical Monitors noticed a spike in grade 3 neutropenia cases from two Eastern European sites. Although these were technically non-serious AEs, the clustering triggered a review. Upon closer inspection, two patients required hospitalization without prior dose adjustments—qualifying them as unreported SAEs.
The Medical Monitor escalated the issue, triggering a targeted site audit and mid-study investigator training. A protocol amendment was issued to add proactive CBC monitoring every three days instead of weekly. This change prevented further escalation and preserved the study timeline without regulatory intervention.
Risk-Based Oversight & Regulatory Compliance
What Is Risk-Based Monitoring (RBM)?
Risk-Based Monitoring (RBM) is a proactive approach that shifts oversight from exhaustive data checking to strategic risk prioritization. Medical Monitors play a critical role by identifying high-risk elements—such as investigational products with narrow safety margins, vulnerable populations, or complex endpoints—and ensuring monitoring efforts focus there.
Unlike traditional 100% source data verification, RBM leverages centralized analytics, remote monitoring tools, and trigger-based alerts to flag deviations or inconsistencies. The monitor must translate these signals into clinical relevance, deciding whether they're indicative of systemic risk or isolated error.
In 2025, RBM is not optional—it’s a regulatory expectation. Monitors are expected to interpret risk signals using real-time dashboards and contribute to the refinement of the trial’s Risk Assessment Categorization Tool (RACT) throughout the study. Their insights guide everything from onsite monitoring schedules to protocol amendments.
Regulatory Standards: ICH-GCP, FDA 21 CFR, EU CTR
Regulatory frameworks shape the boundaries of medical oversight. Medical Monitors must be fluent in ICH-GCP E6(R3), which outlines their role in ensuring patient safety, data accuracy, and ethical conduct. But region-specific laws also apply.
FDA 21 CFR Part 312 & 812 governs investigational drugs and devices in the U.S., mandating expedited reporting of SAEs and monitor involvement in protocol deviations.
EU Clinical Trials Regulation (EU CTR 536/2014) imposes stricter timelines for safety reporting and holds sponsors liable for inadequate oversight.
Other jurisdictions (e.g., PMDA, Health Canada) follow harmonized guidelines but with country-specific inspection patterns, especially for oncology and vaccine trials.
Monitors must document all decisions with references to applicable codes, ensuring inspection readiness across all regions.
Audit Trails & Inspection Readiness
Every oversight action must leave an auditable trail. Medical Monitors are responsible for documenting decisions, queries, and escalations within the trial master file (TMF) or electronic audit logs. This includes rationale for safety signal escalations, justification for tolerating deviations, and actions taken after DMC reviews.
Inspection readiness means anticipating what regulators might ask. For example, why was a known AE not classified as serious at first report? Why was no CAPA implemented after three minor deviations? Monitors must pre-emptively document clinical judgment and risk-benefit analysis to defend their actions.
Common findings in FDA warning letters
Recent FDA inspection data shows recurring issues tied to oversight failures:
Inadequate SAE assessment documentation
Lack of timely protocol deviation follow-up
Missing rationale for continued subject enrollment post-safety flag
These findings underscore the need for rigorous documentation and timely escalation. Medical Monitors who proactively manage these areas reduce inspection risk and reinforce the trial’s scientific integrity.
| Category | Medical Monitor Role | Key Actions / Requirements |
|---|---|---|
| Risk-Based Monitoring (RBM) | Prioritize oversight based on clinical and protocol risk | Use dashboards, RACT tools, trigger-based alerts |
| Traditional vs RBM | Shift from full SDV to centralized, risk-focused monitoring | Identify systemic vs isolated issues with clinical judgment |
| Global Regulatory Standards | Apply international and local frameworks | ICH-GCP E6(R3), FDA 21 CFR 312/812, EU CTR 536/2014 |
| Documentation & Decision Trails | Log oversight decisions, escalations, and justifications | Maintain TMF records and electronic audit logs |
| Inspection Readiness | Anticipate regulatory questions and support findings | Explain AE classifications, deviation handling, CAPAs |
| Common FDA Findings | Prevent repeat inspection failures with robust oversight | Inadequate SAE logs, delayed CAPAs, unclear enrollment rationale |
Collaboration with Sponsors, CROs & Investigators
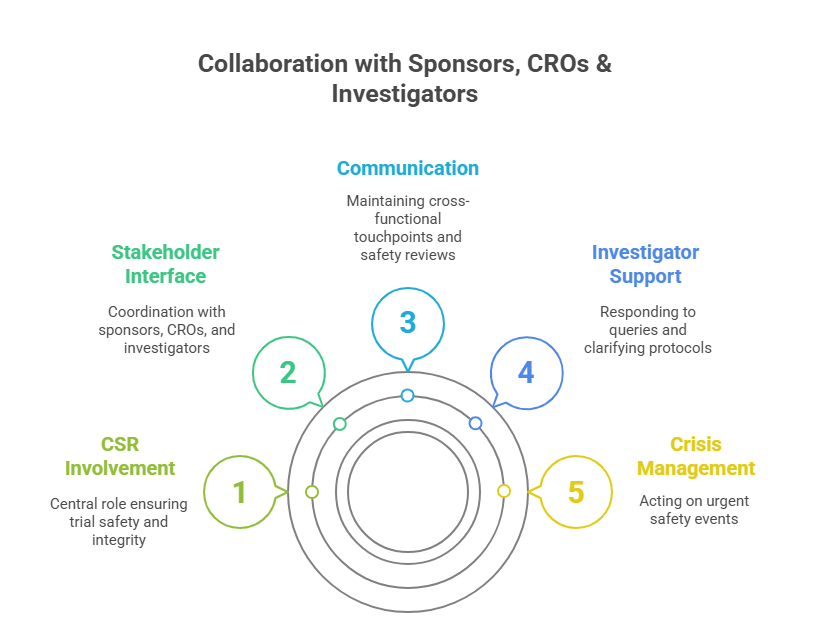
How Medical Monitors Interface Across Stakeholders
Medical Monitors serve as the clinical glue that binds sponsors, CROs, and site investigators. While project managers and CRAs handle logistics and operations, the monitor drives cross-functional clinical alignment. They review site data with medical logic, inform sponsor safety decisions, and ensure that CROs interpret findings within proper clinical context.
Communication is frequent. Monitors join weekly or biweekly cross-functional team (CFT) calls, lead safety reviews, and draft consolidated medical summaries for executive dashboards. Their input is critical during interim analyses, blinded data reviews, and endpoint adjudication discussions.
They also support investigator engagement by reviewing queries, advising on protocol nuances, and flagging trends in adverse event profiles. With decentralized trial models, monitors must be fluent in virtual communication tools and understand cultural nuances across global investigator networks.
Conflict Resolution & Communication Escalation Paths
Clinical trials are high-stakes environments where conflicts often arise—between CROs and sites, or sponsors and investigators. Medical Monitors are often pulled in to resolve disagreements tied to safety assessments, protocol interpretations, or AE classifications.
For example, an investigator might classify a hospitalization as unrelated, while the monitor identifies causality based on pattern recognition. In such cases, the monitor drafts a medical rationale document, aligns with the pharmacovigilance team, and presents it during escalation meetings.
Escalation follows structured paths: monitor to CRO lead → sponsor medical director → independent adjudication committee, if applicable. What separates a strong monitor is the ability to mediate while maintaining regulatory and ethical clarity. Poorly handled escalations risk regulatory misalignment, trial delays, or site dropout.
Who Takes Final Oversight Decisions?
Medical Monitors do not always have the final say—but their recommendations carry weight. In most global trials, final medical oversight decisions rest with the sponsor’s Medical Director or Chief Medical Officer (CMO). However, the monitor’s clinical evaluations often form the basis of that decision.
In urgent cases (e.g., a subject death or unblinded finding), the Medical Monitor’s preliminary input is used to trigger temporary study holds, data locks, or regulatory notifications. Their documentation, provided within 24–48 hours, becomes part of the official safety dossier.
Monitors also advise during final Clinical Study Report (CSR) drafting, ensuring that safety narratives reflect accurate medical judgment and regulatory consistency. While sponsors sign off on the final language, monitors craft the foundational interpretations regulators will read.
Tools & Tech Used in Oversight (CTMS, EDC, Signal Detection)
CTMS Platforms: Medidata, Veeva, & Oracle
Clinical Trial Management Systems (CTMS) are the backbone of centralized oversight operations. Medical Monitors rely on platforms like Medidata Rave CTMS, Veeva Vault CTMS, and Oracle Siebel Clinical to access, analyze, and annotate data across multiple sites in real time.
Each CTMS aggregates subject profiles, adverse event logs, deviation reports, and monitoring visit outcomes. What matters most to monitors is dashboard configuration—custom KPIs, trend flags, and automated alerts tied to protocol-specific criteria. Veeva, for example, allows configuration of threshold triggers for lab anomalies or protocol violations, enabling real-time escalation.
Integration with other tools (EDC, pharmacovigilance systems) ensures monitors don’t work in silos. A well-integrated CTMS supports audit trail clarity, reducing documentation gaps and accelerating inspection readiness.
Signal Detection Software: Empirica, PV-Works
Medical Monitors use dedicated signal detection software to track emerging risks. Two industry leaders are Oracle Empirica Signal and PV-Works, both of which allow real-time signal aggregation from spontaneous reports, trial data, and historical benchmarks.
These tools perform data mining for disproportionate reporting, enabling monitors to catch patterns that human review might miss. For instance, if a new rash appears at three unrelated sites post-dose escalation, Empirica may flag it as a signal of interest. The monitor then performs clinical triage—determining seriousness, causality, and whether to alert the Safety Review Board.
Signal detection tools are especially critical in oncology, immunology, and first-in-human trials, where unexpected toxicities can appear abruptly.
EDC Integration for Monitoring Dashboards
Electronic Data Capture (EDC) systems like Medidata Rave, Inform EDC, and Veeva EDC feed directly into Medical Monitor dashboards. These dashboards are custom-designed views that consolidate lab values, AE timelines, concomitant medication changes, and CRF queries for each subject.
Monitors rely on smart filtering to prioritize what matters: SAE progression over time, protocol-mandated labs, dose modifications, and deviation trends. The EDC acts as the primary source of truth, and integration ensures that all insights are current and actionable.
Custom reports and trend analysis
Advanced dashboards allow monitors to generate automated safety trend reports, flagging subject clusters with shared symptoms, treatment responses, or noncompliance. Monitors can schedule weekly exports, drill down into specific metrics (e.g., QTc interval shifts in males over 60), and overlay them against protocol norms.
Custom reports are often shared during SMT or CFT meetings. These summaries allow stakeholders to make fast, informed decisions. A good monitor doesn’t just read dashboards—they shape them to reflect the study’s real-world medical complexity.
| Tool Category | Platform/Software | Medical Monitor Use |
|---|---|---|
| CTMS Platforms | Medidata Rave CTMS, Veeva Vault CTMS, Oracle Siebel Clinical | Track subject profiles, AE logs, deviations, and monitoring visit outcomes |
| CTMS Features | Custom dashboards, KPI flags, automated alerts | Trigger real-time escalation for lab anomalies or protocol violations |
| Signal Detection Tools | Oracle Empirica Signal, PV-Works | Aggregate safety data, detect signals across spontaneous reports and trial data |
| Critical Use Cases | Oncology, Immunology, First-in-human trials | Flag clusters and rare toxicities earlier than manual review allows |
| EDC Systems | Medidata Rave, Inform EDC, Veeva EDC | Feed data into dashboards for monitoring SAE timelines, labs, and CRF queries |
| Dashboard Reporting | Custom exports, trend overlays, filterable analytics | Share insights with SMT/CFT teams for data-driven safety decisions |
How Our Medical Monitoring Certification Equips You for Oversight
Medical oversight in 2025 requires far more than just clinical knowledge—it demands regulatory fluency, cross-functional coordination, and tech-savvy judgment. Our Advanced Medical Science Liaison & Medical Monitor Training Certification (AMSLC) is designed to equip professionals with every essential competency needed to succeed in this evolving role.
The program covers a comprehensive set of modules aligned with global standards, including ICH-GCP E6(R3), FDA 21 CFR Part 312/812, EMA safety reporting timelines, and EU CTR implementation protocols. Participants learn to identify safety signals, manage deviations, prepare risk mitigation documentation, and communicate effectively across CROs, sponsors, and regulators.
What sets this certification apart is its emphasis on real-world execution. Candidates work through simulated Phase I–IV trial scenarios, reviewing actual adverse event data, drafting medical queries, and preparing deviation justifications. Each task mirrors the pressures and precision required in real oversight roles.
The curriculum also provides deep dives into clinical data interpretation using EDC and CTMS platforms. You'll learn to triage complex patient narratives, prepare escalation documentation, and generate custom trend analysis reports—skills that translate directly into higher-impact decision-making on real studies.
If you’re ready to step into—or advance within—a medical oversight role, this certification offers the most targeted, up-to-date preparation available.
Frequently Asked Questions
-
A Medical Monitor manages ongoing clinical oversight across multiple sites and countries, focusing on participant safety, protocol adherence, and data integrity. A Clinical Research Physician, in contrast, typically works at the sponsor level and may be involved in protocol design, regulatory submissions, and product strategy. While both roles require medical degrees, the monitor is more operational—reviewing data in real time and responding to safety issues. Clinical Research Physicians are often less involved in daily trial execution. That said, in smaller studies, one person may serve both functions, especially during early-phase development or at biotech companies with limited medical affairs staff.
-
No. While many Medical Monitors hold MD or DO degrees, some roles—especially in post-market surveillance or low-risk therapeutic areas—are open to PharmDs or PhDs with clinical trial oversight experience. Still, most sponsors and CROs prefer physicians due to the role's medical judgment demands. In high-risk indications like oncology or neurology, a licensed physician is often required. However, professionals without MDs can still play a major role as Safety Review Specialists, Medical Writers, or in pharmacovigilance support roles. Earning the Advanced Medical Science Liaison & Medical Monitor Training Certification (AMSLC) can significantly increase your credibility in such cases.
-
Medical oversight is governed by a combination of international and local regulations. Globally, ICH-GCP E6(R3) sets the baseline for good clinical practice. In the U.S., FDA 21 CFR Part 312 and 812 governs investigational drugs and devices. Europe follows EU Clinical Trials Regulation (CTR 536/2014). Monitors must also comply with safety reporting requirements under ICH-E2A, which guides adverse event evaluation and expedited reporting. During inspections, regulators expect all oversight decisions to be documented clearly and aligned with these frameworks. Ignoring any of these regulations can result in FDA Form 483 findings, trial delays, or sponsor penalties.
-
Medical Monitors detect safety trends using a mix of clinical insight, data visualization tools, and predefined thresholds. Most use Signal Detection software (like Oracle Empirica or PV-Works) integrated with EDC data to flag patterns—such as rising liver enzyme levels across cohorts. They also review weekly dashboards for AE frequencies, lab anomalies, and treatment discontinuations. Trend detection isn’t just about stats—it’s about identifying clinically meaningful changes in patient outcomes. Monitors compare trends across sites and arms, then prepare justification for escalation. The ability to spot early signals is essential for preventing regulatory holds or patient harm.
-
Global CROs use a variety of platforms to support medical monitoring. These typically include EDC systems (Medidata Rave, Veeva EDC), CTMS platforms (Veeva Vault, Oracle Siebel Clinical), and Signal Detection tools (Empirica, Argus Safety, PV-Works). Medical Monitors often work with dashboards that pull real-time data from these tools, enabling rapid decision-making. CROs may also use AI overlays for data prioritization. Familiarity with at least two EDC and one CTMS platform is now expected. The AMSLC certification includes case-based training with these tools to prepare candidates for global CRO standards.
-
Salaries for Medical Monitors vary based on geography, experience, and therapeutic area. In the U.S., entry-level monitors can earn $130,000–$160,000 per year, with mid-career professionals earning upwards of $200,000 annually. Monitors specializing in oncology, immunology, or gene therapy often command even higher rates. CRO-based roles typically offer base salary plus performance bonuses, while sponsor-side monitors may receive equity or long-term incentives. Globally, the role is also well-compensated in regions like Europe (especially Germany, UK, Netherlands) and Asia-Pacific (Singapore, Japan, Australia), where biotech investment is high.
-
Yes—but a transition requires clinical depth and regulatory understanding. Clinical Research Coordinators (CRCs) and Clinical Research Associates (CRAs) bring site-level experience and protocol familiarity. To become Medical Monitors, they must build competency in medical data interpretation, signal detection, and ICH regulatory compliance. Pursuing a certification like the AMSLC bridges that gap, especially when paired with physician mentorship or entry-level roles in pharmacovigilance. Some CRAs start by supporting safety reviews or handling medical query triage before stepping fully into a monitoring role. Experience in complex therapeutic areas further boosts the likelihood of transition.
Final Thoughts
Medical Monitors are no longer optional in modern clinical trials—they’re foundational. As trials grow more decentralized and data-driven, sponsors and CROs are demanding oversight professionals who can balance medical judgment, regulatory precision, and tech fluency. This isn’t a passive role—it’s an active leadership position that influences patient safety, protocol viability, and trial success.
Whether you're a physician entering clinical research or a clinical professional moving into higher-responsibility roles, mastering oversight is a career-defining move. The Advanced Medical Science Liaison & Medical Monitor Training Certification (AMSLC) offers the fastest and most comprehensive route to get there. If you’re ready to step into a role where your decisions impact global health outcomes, now is the time to act—with skill, speed, and certification.