Ethical Considerations in Clinical Trials: What Every CRC Should Know
Clinical trials are the backbone of medical advancements, providing crucial data on the safety and effectiveness of treatments. But behind every trial is a strict set of ethical guidelines that ensure the protection of participants' rights, safety, and dignity. If you're a Clinical Research Coordinator (CRC), you hold a critical responsibility in ensuring that every aspect of a clinical trial is conducted ethically. In this comprehensive guide, we’ll dive into the most important ethical considerations in clinical trials that every CRC should know to maintain the highest standards of research integrity.
Why Ethical Considerations Matter in Clinical Trials
Ethics in clinical research isn't just about following rules—it’s about ensuring trust, transparency, and respect for the rights of human participants. Whether it's conducting trials for new medications, therapies, or diagnostic techniques, the ethical standards that govern clinical research safeguard the well-being of volunteers and maintain the integrity of the research process. CRCs are often the first line of defense in ensuring that ethical guidelines are adhered to, and that participants receive adequate protection and care throughout the trial process.
Bonus Read: To learn about the process of becoming a Clinical Research Coordinator, explore the essential steps in our guide on how to become a clinical research coordinator.
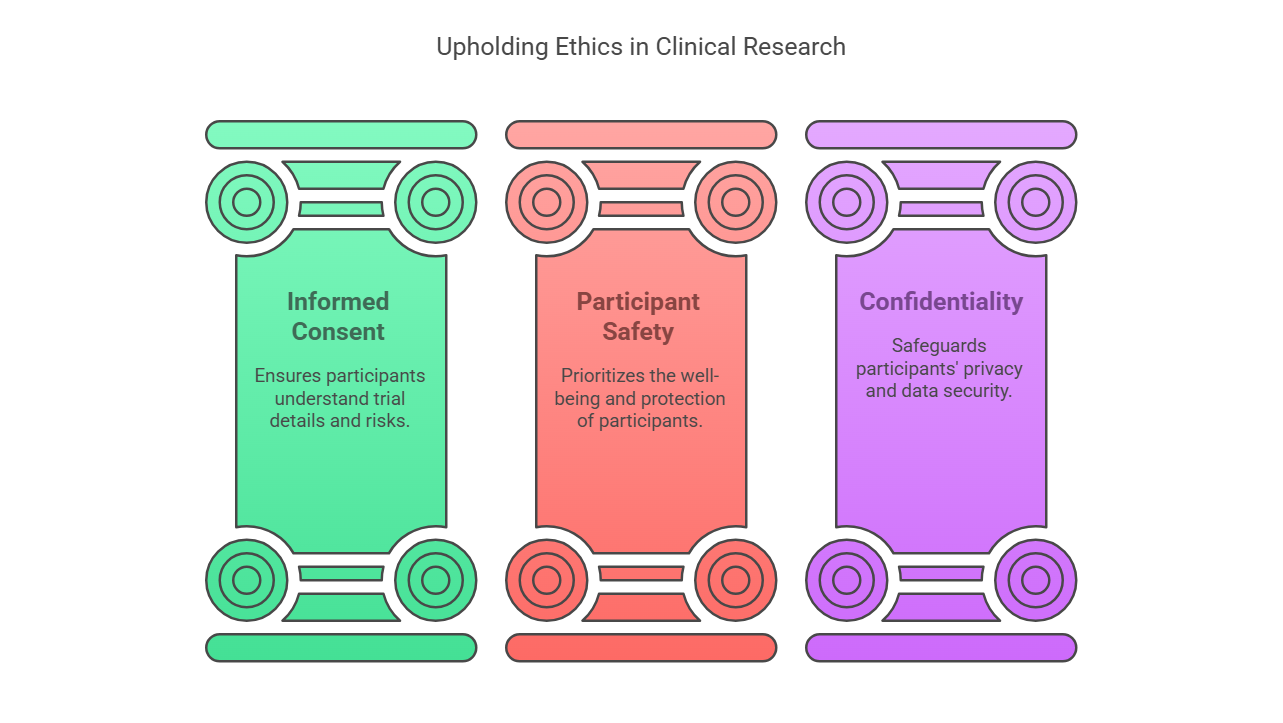
Key Areas of Ethical Consideration:
Informed Consent
The foundation of ethical clinical research is informed consent. Participants must fully understand the trial they are entering, including its potential risks, benefits, and any discomfort they might face. As a CRC, it's your responsibility to ensure that informed consent is obtained and properly documented before the trial begins. You must ensure that all participants comprehend the details of their participation in a language they understand, leaving no room for ambiguity.Participant Safety and Welfare
Throughout the trial, the safety of participants must be a priority. This includes monitoring for adverse events (AEs), managing potential risks, and ensuring that participants are protected from harm. Ethical guidelines require that clinical trials stop if risks outweigh potential benefits. As a CRC, you should be proactive in identifying and mitigating risks to ensure the well-being of every participant involved.Confidentiality and Privacy
Protecting participant privacy is a cornerstone of ethical clinical research. Participants' personal and medical information must be confidential, and research data must be stored securely. The confidentiality of trial participants is safeguarded by laws like HIPAA in the United States and the GDPR in Europe, ensuring that their identities and personal information remain protected throughout the study.
Understanding the full scope of clinical research is crucial for every professional in the field. Learn more about the core aspects in our post on the scope of clinical research and its responsibilities.
Guidelines for Ensuring Ethical Conduct in Clinical Trials
While the ethical framework for clinical research is robust, it’s essential that CRCs actively contribute to upholding these standards throughout the trial process. Below are some key practices every CRC should follow:
Adherence to Regulatory Guidelines
Clinical trials must comply with local, national, and international regulations such as the Declaration of Helsinki, the International Council for Harmonisation (ICH) Good Clinical Practice (GCP), and the U.S. Food and Drug Administration (FDA) regulations. These guidelines help maintain the ethical integrity of the trial. A CRC must ensure that all team members understand and adhere to these protocols to maintain compliance.Ongoing Monitoring and Audits
Routine monitoring and audits are essential to detect any deviations from the ethical standards. Regular assessments help ensure that the trial progresses according to ethical guidelines and regulatory requirements. CRCs play a key role in facilitating audits and making sure that all records are accurate and up to date.Ensuring Voluntary Participation
It is essential that participation in clinical trials is voluntary. Coercion or undue influence is never acceptable. The informed consent process should reinforce the participant's right to withdraw from the trial at any time without penalty. CRCs must be attentive to ensuring that no participant feels pressured into continuing their participation if they are uncomfortable at any stage of the trial.
Common Ethical Issues in Clinical Trials and How to Address Them
Even with stringent ethical guidelines, some common ethical issues can arise in clinical trials. Let’s explore a few examples and how CRCs can address them:
Undue Influence or Coercion
Some participants may feel compelled to join a trial due to financial incentives, social pressures, or the perceived benefits of being in a study. CRCs should actively ensure that consent is voluntary and free from any pressure.Bias in Patient Recruitment
It’s crucial to avoid discrimination in recruitment and ensure that the participant pool is diverse and reflective of the general population. CRCs must ensure the recruitment process is fair and unbiased, offering equal opportunity for all eligible candidates.Failure to Disclose Potential Risks
Sometimes, potential risks of a trial may not be clearly communicated to participants, which can lead to serious ethical violations. CRCs should ensure that every participant is made fully aware of any potential risks and side effects before joining the trial.
The Role of the CRC in Ethical Clinical Trials
As a Clinical Research Coordinator, your role in maintaining ethical standards is vital. From managing the logistics of the trial to ensuring that ethical guidelines are followed at every step, CRCs are instrumental in safeguarding the integrity of clinical research.
Provide Continuous Education and Training: Ensuring that all team members are continually trained on the ethical aspects of clinical trials helps prevent ethical breaches. Regular refresher courses on GCP informed consent and participant safety should be mandatory.
Monitor and Report Ethical Breaches: CRCs are often the first to spot potential ethical issues. Reporting concerns promptly can prevent harm to participants and ensure that the trial continues to meet ethical standards.
Act as a Liaison Between the Research Team and Participants: CRCs are in constant communication with both the research team and trial participants, helping to clarify any doubts participants may have and ensuring they remain informed.
Conclusion
Ethical considerations in clinical trials are crucial for ensuring the protection of participants and the integrity of the research. As a CRC, you hold an essential role in upholding these ethical standards, ensuring that the trials you coordinate are conducted with the highest degree of responsibility and respect for human rights. By staying informed and vigilant, CRCs can help ensure the success and ethical compliance of clinical trials, paving the way for new medical breakthroughs that benefit all of society.
If you’re looking to enhance your career in clinical research and gain a deeper understanding of the ethical and regulatory frameworks that guide the industry, consider earning your certification through CCRPS. With specialized training in clinical research, you’ll be better equipped to navigate ethical challenges in your trials and contribute to advancing science with integrity.
-
Informed consent is the most fundamental ethical principle, ensuring participants understand the risks and benefits before joining a trial.
-
CRCs monitor adverse events, manage risks, and ensure that participant safety is always prioritized throughout the trial process.
-
Protecting participant privacy ensures that sensitive personal and medical data remains secure and that individuals' rights are respected.
-
The CRC ensures ethical guidelines are followed, addresses any concerns raised by participants, and reports any deviations from ethical standards.
-
It ensures participants are fully aware of the study’s objectives, potential risks, and benefits, allowing them to make an informed decision.
-
Common issues include coercion, failure to disclose risks, and biased recruitment practices. CRCs must be vigilant to address these issues promptly.
-
By ensuring compliance with ethical guidelines, monitoring participant safety, and maintaining transparent communication with the research team.
-
Unethical practices can lead to the invalidation of trial results, harm to participants, and damage to the credibility of the research institution.