Top 20 Must-Know Terms for Clinical Trial Project Managers PMs
Clinical Trial Project Managers (PMs) stand at the critical crossroads of regulatory compliance, trial efficiency, and stakeholder communication. In an industry where each term carries regulatory weight and operational significance, understanding the most crucial terms isn’t optional—it’s essential. Precision in terminology directly impacts trial success, from ensuring correct Good Clinical Practice (GCP) adherence to safeguarding data integrity during audits. This guide distills the top 20 must-know terms every PM must master, providing a laser-focused resource to strengthen operational clarity, elevate communication with regulatory bodies, and minimize costly errors. Mastery of these terms ensures PMs can lead with authority, anticipate compliance risks, and navigate complex regulatory landscapes with confidence.
This isn’t just a vocabulary list—it’s a survival toolkit for ambitious Clinical Trial PMs. Whether collaborating with CROs, preparing for an FDA audit, or reporting to stakeholders, knowing these terms gives you the edge. Each definition is built for clarity, and designed to embed directly into your operational vocabulary. Let’s dive deep into this indispensable knowledge base and equip you for clinical trial project management excellence.
The Power of Clinical Trial Terminology
Clinical trials are driven by language. For Clinical Trial Project Managers (PMs), precision in terminology is not just an operational necessity; it is a strategic asset that directly impacts compliance, communication, and trial outcomes. A single ambiguous term can derail a project’s timeline, misinform stakeholders, or even trigger regulatory penalties. Conversely, accurate terminology enables PMs to anticipate compliance challenges, navigate Good Clinical Practice (GCP) frameworks, and communicate seamlessly across cross-functional teams.
In an environment where clinical trials intersect with strict regulations and high-stakes data management, terminology is power. It builds the foundation for clear protocols, consistent documentation, and smooth interactions with regulatory bodies such as the FDA and EMA. Every term holds operational weight, and precision ensures that all team members—from data managers to monitors—stay aligned with project goals.
Why Precision Matters
Precise language eliminates ambiguity. For instance, a Source Data Verification (SDV) note must be unmistakably clear to pass audits and avoid compliance issues. Terminology consistency reduces the risk of misinterpretation and supports CROs and sponsors in executing projects flawlessly. It also ensures seamless communication during site visits and monitoring. PMs who master precise language gain credibility, enabling them to manage escalations proactively and maintain trial momentum.
How These Terms Impact Compliance and Communication
Terminology is the bridge between operational execution and regulatory compliance. For example, the difference between Adverse Event (AE) and Serious Adverse Event (SAE) can determine reporting obligations and trial risk assessment. Using the correct term aligns with regulatory expectations and prevents delays in approvals or escalations. Additionally, precise terminology enhances communication between stakeholders—whether internal teams, regulatory authorities, or site staff. Miscommunication at this level isn’t a minor issue—it can jeopardize the trial’s integrity. PMs equipped with a precise, standardized vocabulary can confidently manage complex documentation, resolve issues faster, and deliver successful outcomes.
Essential Terms Table: The Top 20 Must-Know Terms for PMs
Understanding critical clinical trial terms isn’t just about speaking the language—it’s about maintaining compliance, ensuring data integrity, and aligning operational decisions with global regulatory standards. This curated list provides clear, precise definitions of essential terms every Clinical Trial Project Manager (PM) must master. Each term is not only foundational for daily trial operations but also for seamless communication with regulatory bodies, ensuring projects run smoothly and deliver reliable results. This table is your quick-reference guide to the vocabulary that drives success in complex clinical trials.
| Term | Definition |
|---|---|
| 1. Good Clinical Practice (GCP) | International quality standard ensuring ethical and scientifically sound trials. Defines roles, responsibilities, and standards for data integrity, patient safety, and regulatory compliance. |
| 2. Investigational Product (IP) | Drug, biologic, or device under investigation in a clinical trial. Includes the placebo and comparator products, critical for blinding and treatment assessments. |
| 3. Adverse Event (AE) | Any untoward medical occurrence in a participant during a trial, regardless of its relationship to the investigational product. Essential for safety reporting. |
| 4. Serious Adverse Event (SAE) | An AE resulting in death, hospitalization, or life-threatening conditions. Requires immediate reporting and impacts trial risk assessments. |
| 5. Case Report Form (CRF) | Standardized document for collecting trial data per protocol. Supports data integrity, traceability, and compliance with regulatory standards. |
| 6. Source Data Verification (SDV) | Cross-checking CRF data against original source documents to ensure accuracy and completeness for regulatory inspections. |
| 7. Clinical Trial Protocol | Formal plan outlining study objectives, methodology, statistical considerations, and organization. Approved by regulatory authorities and ethics committees. |
| 8. Informed Consent Form (ICF) | Document ensuring participants’ understanding of trial risks and procedures. Obtained before trial participation and maintained throughout the study. |
| 9. Institutional Review Board (IRB) | Ethics committee responsible for safeguarding participant rights, safety, and well-being during clinical trials. |
| 10. Clinical Trial Management System (CTMS) | Software platform managing trial planning, tracking, and reporting. Streamlines data management and enhances operational efficiency. |
| 11. Monitoring Plan | Comprehensive plan detailing monitoring strategies, responsibilities, and processes for ensuring protocol and regulatory compliance. |
| 12. Data Management Plan (DMP) | Document outlining procedures for data handling, processing, and validation to maintain integrity and accuracy. |
| 13. Randomization | Process of assigning participants to treatment groups using chance to minimize bias. Essential for statistical validity. |
| 14. Blinding | Concealing treatment allocation from participants and/or researchers to prevent bias. Critical for maintaining trial objectivity. |
| 15. Audit Trail | Electronic or manual record of data changes, ensuring traceability, accountability, and compliance with regulations. |
| 16. Deviation | Departure from the approved protocol or GCP standards. Requires documentation and potential corrective action to maintain trial validity. |
| 17. Electronic Data Capture (EDC) | Digital system for collecting and managing clinical trial data in real-time, enhancing efficiency and compliance. |
| 18. Serious Breach | A violation of GCP or protocol significantly affecting participant safety or data integrity. Must be reported to regulatory authorities. |
| 19. Pharmacovigilance | Ongoing safety monitoring of investigational products, including adverse event detection, reporting, and risk management. |
| 20. Clinical Study Report (CSR) | Comprehensive report summarizing trial methodology, results, and conclusions. Submitted to regulatory authorities for approval and publication. |
Key Regulatory and Compliance Insights for PMs
Clinical Trial Project Managers (PMs) must be fluent in regulatory frameworks to ensure trial integrity, patient safety, and operational excellence. Regulatory and compliance knowledge isn’t theoretical—it’s a core operational necessity. Mastery of guidelines like Good Clinical Practice (GCP) and frameworks from authorities like the FDA, EMA, and MHRA is what differentiates a compliant trial from one at risk of failure.
Navigating GCP and ICH Guidelines
GCP is the backbone of ethical and scientifically sound trials. It outlines how PMs should handle everything from informed consent forms to adverse event reporting. Non-compliance can trigger regulatory investigations and jeopardize entire projects. The International Council for Harmonisation (ICH) guidelines complement GCP by standardizing protocols across global trials. For PMs, this means knowing ICH’s E6(R2) and related updates inside out—ensuring that monitoring plans, data management, and site operations align with both local and international expectations. Regulatory harmonization isn’t optional; it’s what allows multi-country trials to succeed.
The Role of Regulatory Bodies
Regulatory bodies like the FDA, EMA, MHRA, and PMDA play critical roles in trial approvals, monitoring, and post-marketing surveillance. Their expectations are clear: compliance with GCP, ethical considerations, accurate data reporting, and participant protection. PMs must know submission pathways (e.g., INDs, CTAs), understand local variations (e.g., Europe’s GDPR requirements), and anticipate audits. They must also implement real-time compliance monitoring—ensuring timely reporting of serious adverse events (SAEs) and maintaining robust documentation for inspection readiness. Proactive PMs align operations with regulators, transforming compliance from a reactive burden to a strategic advantage.
Regulatory fluency isn’t just about passing inspections—it’s about safeguarding the trial’s credibility, protecting participants, and ensuring timely market approvals. PMs who anticipate regulator expectations, train teams in compliance protocols, and maintain meticulous records are the ones who lead high-performing, audit-ready trials.
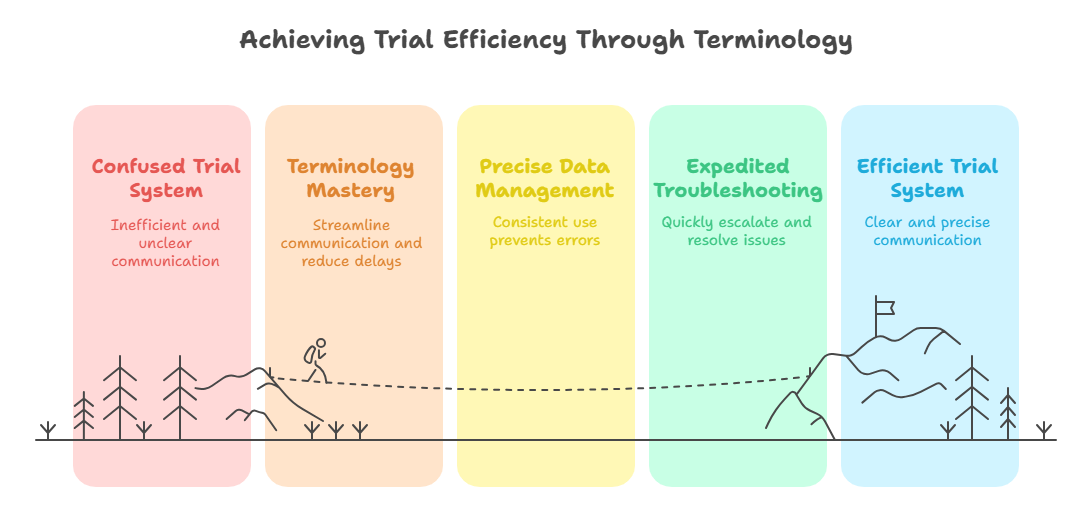
Strengthening Trial Efficiency Through Terminology Mastery
Clinical Trial Project Managers (PMs) don’t just manage timelines—they orchestrate complex systems where efficiency hinges on precision and shared understanding. Terminology mastery streamlines communication, minimizes delays, and enhances data quality, driving project success. Each term used in meetings, reports, or protocols holds operational weight, and its proper application directly impacts efficiency.
From Site Monitoring to Data Management
Site monitoring isn’t just a checklist exercise; it’s about ensuring compliance and data integrity through precise terminology. For instance, consistent use of terms like Source Data Verification (SDV) and Deviation clarifies site issues and expedites resolutions. Mislabeling a Serious Adverse Event (SAE) or using inconsistent definitions in reports can delay corrective actions and risk regulatory penalties. Similarly, in data management, clarity in terms like Case Report Form (CRF) and Electronic Data Capture (EDC) enhances accuracy and accelerates data reconciliation. PMs who enforce standard terminology not only prevent errors but also enable cross-functional teams to collaborate more effectively.
Troubleshooting with Precision
When issues arise—be it discrepancies in participant data, protocol deviations, or unexpected site challenges—PMs who command precise terminology can troubleshoot faster and more effectively. For example, distinguishing between a Serious Breach and a routine Deviation determines escalation pathways and reporting requirements. Knowing these distinctions in real time saves valuable hours, prevents compounding errors, and ensures the trial remains on track.
Moreover, precise terminology transforms cross-team communication. Instead of vague descriptions, a PM can instruct a site to correct a GCP-related discrepancy or clarify a DMP update without ambiguity. This level of precision not only boosts operational efficiency but also demonstrates a commitment to regulatory excellence.
PMs who master these terms don’t just keep projects moving—they lead with authority, resolve issues faster, and set the gold standard for clinical trial management efficiency.
Enhancing Stakeholder Communication
In clinical trials, precise terminology isn’t just about internal operations—it’s the backbone of clear, credible communication with all stakeholders. Clinical Trial Project Managers (PMs) who use standardized terms ensure that cross-functional teams, regulatory bodies, and sponsors receive consistent, actionable information. Every report, meeting, and stakeholder update becomes a chance to reinforce trust and maintain alignment.
Using the Right Terms in Reports and Meetings
Stakeholder communication isn’t about simplifying complex data—it’s about making it clear and precise. When PMs use terms like Clinical Study Report (CSR), Monitoring Plan, and Informed Consent Form (ICF) correctly, they convey professionalism and regulatory readiness. Consistent terminology across reports ensures that findings are transparent and defensible during inspections or audits. In meetings, the right terms expedite decisions, minimize misinterpretations, and build stakeholder confidence. For instance, clarifying the distinction between an AE and an SAE can change the course of a safety discussion.
Avoiding Misunderstandings with Precise Language
Misunderstandings cost time, money, and credibility. An incorrect term in a report or an ambiguous statement during a regulatory meeting can delay approvals or trigger follow-up inquiries. Precise terminology prevents these risks. When a PM clearly defines a Deviation, specifies its impact, and proposes corrective actions, the response from stakeholders is immediate and focused. Moreover, using globally recognized terms—aligned with GCP and ICH—facilitates communication across international sites and regulatory landscapes.
PMs who consistently apply precise language establish themselves as credible leaders. They not only ensure that their trials stay on track but also that every stakeholder—be it a CRO, sponsor, or regulatory agency—has complete confidence in the project’s integrity.
| Section | Key Points |
|---|---|
| Enhancing Stakeholder Communication |
|
| Key Benefit: Clarity and Consistency |
|
| Critical Skill: Distinguishing Terms |
|
| Risk Mitigation: Avoiding Misunderstandings |
|
| Outcome |
|
Elevate Your PM Career with the CCRPS Clinical Research Manager Certification
For Clinical Trial Project Managers (PMs), mastering terminology and regulatory nuances isn’t just about keeping projects on track—it’s a career-defining skill. The CCRPS Clinical Research Manager Certification is the definitive pathway to elevate your expertise, positioning you as an indispensable leader in clinical research.
This advanced certification program is meticulously designed to deepen your command of GCP standards, regulatory frameworks, and operational excellence. Through immersive modules and real-world case studies, PMs not only learn terminology but also how to apply it effectively in global trials. The certification covers advanced concepts like managing serious breaches, designing data management plans (DMPs), and aligning trial operations with FDA and EMA expectations.
Graduates of the CCRPS Clinical Research Manager Certification emerge with the confidence to lead complex, multi-site trials. The program empowers them to communicate seamlessly with stakeholders, preempt compliance challenges, and navigate audits with ease. In an era where clinical trials are increasingly globalized and regulated, this certification distinguishes PMs who can deliver compliant, efficient, and high-quality results.
Advanced training modules ensure PMs master the precise use of terms like Electronic Data Capture (EDC), Case Report Form (CRF), and Clinical Study Report (CSR)—each integral to data accuracy and regulatory success. With this certification, PMs gain tools to enhance communication, reduce operational risks, and increase trial efficiency.
Enrolling in the CCRPS Clinical Research Manager Certification is more than a professional upgrade—it’s a strategic investment in career advancement. Certified professionals demonstrate readiness to lead in high-stakes environments, ensuring trial success and bolstering their marketability.
Frequently Asked Questions
-
Clinical Trial Project Managers (PMs) often encounter challenges like ensuring GCP compliance, adapting to evolving ICH guidelines, and managing international regulatory variations. Navigating complex reporting obligations—especially for SAEs, protocol deviations, and data discrepancies—demands precision and proactive oversight. PMs must stay updated on region-specific requirements (e.g., GDPR in Europe, 21 CFR Part 11 in the U.S.) and anticipate regulatory audits. Misinterpretation of terms or reporting delays can trigger penalties or trial disruptions. Effective PMs implement real-time compliance monitoring, robust documentation strategies, and regular stakeholder training to overcome these challenges and maintain trial integrity.
-
Terminology mastery ensures precise communication and uniform data interpretation across global sites. For example, clear distinctions between an Adverse Event (AE) and a Serious Adverse Event (SAE) impact reporting obligations and data categorization. Consistent use of terms like EDC, CRF, and Monitoring Plan reduces ambiguity in documentation, enhances traceability, and supports accurate data reconciliation. When PMs use standardized terminology, cross-functional teams can collaborate effectively, reducing data discrepancies and minimizing costly rework. This clarity safeguards data integrity, supports faster approvals, and ultimately improves patient safety outcomes.
-
GCP compliance is the bedrock of ethical, reliable clinical trials. It ensures patient protection, data accuracy, and adherence to regulatory expectations. For PMs, non-compliance risks trial suspension, fines, or reputational damage. GCP sets clear standards for informed consent, data management, and safety reporting, guiding every operational aspect. Mastering these standards empowers PMs to align cross-functional teams, anticipate regulatory challenges, and ensure trial readiness for inspections. By integrating GCP principles into daily operations, PMs protect participant welfare and support robust, actionable clinical data for regulatory submissions.
-
Preparation for regulatory audits starts with comprehensive documentation, precise terminology, and proactive issue resolution. PMs should ensure that monitoring reports, CRFs, and audit trails are complete, accurate, and aligned with GCP standards. Regular internal audits help identify gaps early. PMs must also train teams on compliance protocols, ensuring all site and operational staff understand regulatory expectations. Clear, precise communication with CROs and vendors ensures readiness for cross-audits. Maintaining a real-time compliance dashboard and conducting mock inspections can further reinforce preparedness and boost confidence during official audits.
-
A protocol deviation is a minor, often isolated, departure from trial protocols or GCP standards, typically without significant impact on participant safety or data integrity. In contrast, a serious breach is a major violation that materially affects participant rights, safety, or data credibility. Serious breaches must be reported to regulatory authorities and may halt the trial until corrective actions are implemented. PMs need to distinguish these to apply appropriate escalation procedures, maintain compliance, and safeguard trial continuity. Precision in terminology during documentation ensures the right regulatory pathways are followed.
-
The CCRPS Clinical Research Manager Certification equips PMs with deep operational knowledge and precise terminology mastery. It offers comprehensive training in GCP, ICH guidelines, data management, and stakeholder communication. PMs gain advanced skills to lead global trials, anticipate regulatory issues, and manage complex operational challenges. The certification enhances credibility with employers and regulatory bodies, boosts career prospects, and prepares PMs to handle real-world trial complexities. Graduates emerge ready to deliver compliant, efficient, and successful clinical trials, elevating their professional profile and marketability.
-
Regulatory requirements vary significantly across regions, adding complexity to global trials. For instance, GDPR in Europe impacts data privacy, while the FDA in the U.S. has specific submission pathways like INDs. PMs must align trial processes with local standards, ensuring consistency in documentation, participant consent, and reporting. Understanding region-specific nuances, such as timelines for SAE reporting or requirements for IRB approvals, is critical. PMs who master these differences minimize delays, prevent compliance issues, and facilitate smoother global trial execution.
Conclusion
In the complex world of clinical trials, Clinical Trial Project Managers (PMs) are the linchpins of operational success, regulatory compliance, and stakeholder confidence. Mastering critical terminology isn’t just a skill—it’s a strategic asset that empowers PMs to lead with authority, mitigate risks, and drive trial efficiency. This guide has armed you with the top 20 must-know terms, regulatory insights, and proactive communication strategies that define high-performing PMs in today’s global research landscape.
Whether you’re preparing for your next GCP audit, optimizing data accuracy with precise terminology, or elevating your career with the CCRPS Clinical Research Manager Certification, every word you use counts. Precision, clarity, and regulatory fluency aren’t optional—they’re essential to navigating trials successfully and safeguarding participant safety.
Stay sharp, keep learning, and position yourself as the PM who not only knows the language of clinical research but masters it.
| Poll: What is the biggest challenge you face as a Clinical Trial PM? | |
| Navigating complex regulations | |
| Managing site compliance | |
| Communicating with stakeholders | |