Clinical Trial Documentation under GCP: Comprehensive Guide
In clinical research, documentation isn’t admin overhead—it’s the foundation of regulatory compliance. Every consent form, protocol version, and data point must be recorded in a way that’s auditable, contemporaneous, and verifiable. Regulatory authorities like the FDA, EMA, and MHRA require documentation to support both the safety of participants and the integrity of the data collected.
This guide delivers a focused breakdown of how Good Clinical Practice (GCP) principles govern clinical trial documentation. You’ll understand which essential records must be maintained, how electronic systems are transforming traditional processes, and the most common reasons trials fail audits. We’ll also explore the demands of global trials, how sponsor and site responsibilities are split, and how the CCRPS Good Clinical Practice (GCP) Certification equips professionals to meet documentation standards across regions.
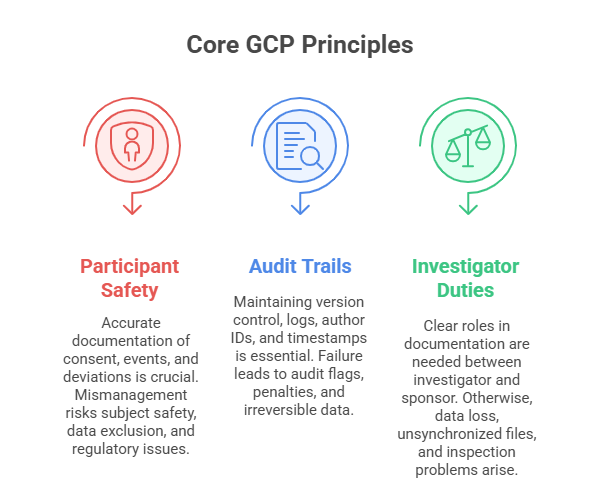
Core Principles of GCP That Affect Documentation
Participant Safety & Data Integrity
At the heart of GCP lies participant protection and uncompromised data quality. Documentation must demonstrate that each participant was informed, consented, and treated ethically throughout the trial. It must also verify that collected data is complete, accurate, and reflects what actually occurred. Regulators expect every adverse event, treatment deviation, or protocol change to be documented in a way that proves subject safety was never jeopardized. Poor documentation around these points can lead to disqualification of data or entire trial sites. Ensuring source data aligns with the CRFs and audit records isn’t a formality—it’s a legal safeguard.
Audit Trails and Traceability
GCP documentation must allow auditors and inspectors to trace every decision, change, and entry back to its origin. This traceability requires precise version control, proper storage of historical records, and real-time updates to logs like the Delegation of Authority or Screening Logs. Electronic records must also include tamper-proof audit trails, with clear timestamps and author identification for every change. Any lapse in traceability—like missing metadata or unexplained overwrites—can trigger audit flags, regulatory findings, or sponsor termination. Traceability is not just about transparency; it’s about building defensible documentation.
Responsibilities of Investigators and Sponsors
Under GCP, both investigators and sponsors share documentation duties—but their responsibilities are distinct. Investigators are accountable for source documentation, informed consent forms, protocol adherence logs, and any site-level logs or correspondence. Sponsors, on the other hand, must maintain the Trial Master File, ensure document completeness across all sites, and verify document accuracy during monitoring visits. GCP mandates that both parties maintain clear lines of accountability, and any overlap—like correspondence or safety reports—must be duplicated across both the sponsor and site files. Failure to separate or synchronize responsibilities results in misfiled data and incomplete records.
Essential Document Categories in Clinical Trials
Investigator Site Files (ISF)
The Investigator Site File (ISF) is the primary documentation repository at the site level. It holds records that prove the trial was conducted per protocol and regulatory requirements. Essential documents include delegation logs, signed informed consent forms, training records, and site correspondence. These aren’t just organizational tools—they’re legal proof of compliance. Inspectors often start audits by reviewing the ISF, and missing documents here can invalidate a site's data. Site staff must maintain the ISF in real-time, not retroactively, with each document version signed, dated, and filed as per the sponsor’s master list.
Trial Master File (TMF)
The Trial Master File is the sponsor’s comprehensive archive for the study, consolidating documents from all participating sites. It includes monitoring visit reports, contracts, central lab certifications, and regulatory authority communications. According to ICH-GCP E6(R2), the TMF must allow trial conduct to be reconstructed and verified independently at any stage. Sponsors may use paper, hybrid, or electronic TMFs (eTMF), but all versions must meet audit-readiness standards. The TMF structure is often aligned to the DIA Reference Model, and gaps in TMF completeness are one of the top reasons for inspection findings.
Regulatory Documents and SOPs
Regulatory files include key documents like the clinical trial application (CTA), ethics committee approvals, IRB submissions, and financial disclosures. These documents serve as proof of regulatory authorization and ethical oversight. Every approval must be version-controlled, signed, and archived in both the ISF and TMF where applicable. Alongside these, site and sponsor Standard Operating Procedures (SOPs) define how each document is created, updated, reviewed, and archived. SOP noncompliance—such as outdated logs or unsigned amendments—can trigger critical Good Clinical Practice violations during audits or FDA inspections.
Source Documentation & CRFs
Source documentation refers to the original data points recorded during the trial—vital signs, lab results, imaging, patient diaries—and must be maintained in a legible, permanent, and retrievable format. These records are the raw truth of the trial and must align exactly with what’s reported in Case Report Forms (CRFs). CRFs are the sponsor’s tool for data collection and submission, and discrepancies between CRFs and source records lead to data integrity concerns. Any correction to either must be dated, signed, and justified per ALCOA+ principles: Attributable, Legible, Contemporaneous, Original, Accurate, plus Complete and Enduring.
Electronic vs. Paper Documentation: Best Practices
FDA Part 11 and EMA eTMF Guidelines
If you're using electronic systems in a clinical trial, FDA 21 CFR Part 11 and EMA’s eTMF guidance are non-negotiable. Part 11 requires that all electronic records be trustworthy, secure, and equivalent to paper—this includes validation, audit trails, user authentication, and record retention. The EMA’s eTMF guidelines further emphasize that eTMFs must be accessible to inspectors during site visits and remain readable throughout their entire retention period. Ignoring these standards doesn’t just increase compliance risk—it can render entire trials non-inspectable, especially if digital documentation lacks system validation or audit trail capabilities.
Security, Accessibility, and Redundancy Planning
Electronic documentation demands a balance between usability and protection. Systems must enforce role-based access, encryption, and secure logins—without making day-to-day usage burdensome for trial staff. Just as importantly, sites must have redundancy protocols in place, including automatic backups and disaster recovery plans. Loss of data due to system crashes, expired cloud access, or permission misconfigurations is no longer an acceptable excuse during audits. In global multicenter trials, failure to ensure document accessibility across regions—whether due to firewalls, broken links, or platform outages—jeopardizes real-time oversight and data reliability.
Common Digital Errors That Trigger Audit Flags
Most inspection findings related to e-documents stem from avoidable operational errors. These include overwriting entries without audit trails, retroactively signing documents, or failing to deactivate access after staff departure. Many systems log data invisibly—making it easy to miss unauthorized edits or backdated signatures. Others lack timestamp granularity, leading to non-compliance with GCP expectations. Even missing document metadata—like who uploaded a file or when—can flag systems as non-validated. To prevent these issues, clinical teams must combine proper software validation with SOP-driven digital behaviors, including routine quality checks and role-specific documentation training.
| Key Focus Area | Best Practices & Risks |
|---|---|
| FDA Part 11 and EMA eTMF Guidelines | Systems must comply with 21 CFR Part 11 and EMA’s eTMF guidance. This includes validated audit trails, user authentication, and long-term accessibility. Non-compliance can result in trials being deemed non-inspectable. |
| Security, Accessibility, and Redundancy | Implement role-based access, data encryption, and auto-backups. Redundancy protocols are essential to avoid data loss from system crashes or expired cloud storage. In global trials, lack of access across regions can compromise oversight. |
| Common Digital Errors | Frequent issues include overwritten data without audit trails, inactive user accounts, and missing metadata. These errors flag systems as non-validated. Preventive measures include software validation and SOP-enforced documentation behavior. |
Common Compliance Pitfalls and How to Avoid Them
Incomplete Signatures or Missing Logs
One of the most frequent findings in clinical audits is incomplete delegation logs or unsigned documents. Every investigator, sub-investigator, or coordinator involved in a task must be documented on the Delegation of Authority log—with initials, roles, dates, and signatures. Similarly, essential logs like IP accountability, screening, and consent must be complete, contemporaneous, and cross-verified. Missing or partially filled logs invalidate entire data streams, especially when tied to adverse events or unblinded visits. A signed form isn’t enough—it must match the site’s staffing timeline and training records. Without this consistency, sponsors and regulators treat it as a GCP documentation failure.
Deviations Not Reflected in Source Documents
Every protocol deviation—whether minor or major—must be recorded in both the source documents and reported through sponsor systems. One of the most overlooked pitfalls is failing to document the root cause and corrective actions. Even when the deviation is reported in an email or safety log, omission from the actual subject chart constitutes a data integrity breach. Auditors check that the source notes, CRF, and deviation log align. If the reason for the deviation or follow-up is vague or missing, it signals that the site lacks protocol oversight, which is a red flag for regulatory bodies like the FDA or EMA.
Lack of Version Control on Protocol Amendments
Failure to control protocol versions results in catastrophic compliance errors. Each amendment must be clearly tracked, signed, dated, and implemented across all documents and systems. Using outdated versions—whether for consent forms, lab manuals, or eligibility criteria—can invalidate subject enrollment or even compromise safety. Sites must retain a master log of protocol versions and prove when each version was adopted. Mixing versions during a single visit, or uploading an amendment without site training documentation, violates ICH-GCP and often leads to findings in both sponsor and site files. Protocol version control is not optional—it’s a regulatory trigger.
| Compliance Pitfall | Description & Risks |
|---|---|
| Incomplete Signatures or Missing Logs | Delegation logs, consent forms, and accountability logs must be fully signed, dated, and aligned with staffing records. Missing entries can lead to invalidated data and GCP compliance failures during audits. |
| Deviations Not in Source Documents | All protocol deviations must be reflected in source documents, CRFs, and deviation logs. Missing root causes or vague follow-ups trigger data integrity breaches and raise red flags for regulators. |
| Lack of Version Control | Every protocol amendment must be tracked, implemented, and version-controlled. Using outdated versions during visits leads to invalid data, regulatory findings, and subject safety risks. |
Documentation in Multicenter and Global Trials
Language and Localization Requirements
In global trials, documentation must meet local language requirements for both regulatory authorities and participant-facing materials. Informed consent forms, subject diaries, and safety reporting tools must be translated into the regional language—and back-translated to verify accuracy. Failure to localize documents accurately can result in ethical violations or trial suspension. Regulatory bodies in countries like Japan, Germany, and Brazil routinely reject documents that aren’t natively accessible. Equally important is ensuring version synchronization: if a new protocol or consent form is released in English, translated versions must match line-by-line in content and formatting across all active sites.
Country-Specific Regulatory Differences
Each participating country enforces unique documentation standards. For example, India requires audio-visual consent recording, while Canada demands storage compliance with PIPEDA, not just GDPR. These nuances go beyond formatting—they affect how data is collected, who must sign off, and how long documents are retained. In some regions, ethics committee approvals must be obtained at the institutional, not central, level. Without a country-specific regulatory matrix, sponsors risk noncompliance despite strong documentation elsewhere. Coordinating teams must stay updated on regulatory circulars, local legislation changes, and import/export requirements for essential documents.
Coordinating Central vs. Site-Level Records
One of the most complex aspects of multicenter trials is maintaining synchronized central and site-level files. The sponsor’s Trial Master File (TMF) must match the documentation held in each site's ISF—not just in content, but in date, version, and filing logic. Discrepancies—such as a site using an outdated SAE reporting form—can reflect a failure of sponsor oversight. Sponsors must implement standardized filing structures (often aligned with the DIA model) and deploy remote monitoring to reconcile gaps in real time. Without that, documentation fragmentation becomes a compliance liability across all trial sites.
How CCRPS Certification Covers Clinical Trial Documentation
The Good Clinical Practice Certification offered by CCRPS is built for clinical professionals who need operational mastery over GCP documentation standards. This isn't a surface-level overview—it’s a course engineered around real regulatory expectations, including FDA 21 CFR Part 11, ICH E6(R2), and EMA inspection guidelines. Whether you're coordinating source documents at site level or overseeing TMF consistency as a sponsor, the certification ensures that your approach is compliant, audit-ready, and globally aligned.
Mastery of ISF and TMF Management
The certification includes full modules on both Investigator Site File (ISF) and Trial Master File (TMF) structure, version control, reconciliation, and audit readiness. It teaches professionals how to implement sponsor-approved TMF reference models, manage investigator correspondence logs, and set up SOP-based filing hierarchies. These lessons go far beyond theory—they walk learners through real inspection findings, showing how document misalignment between sponsor and site gets flagged. You’ll also gain guidance on cross-site TMF tracking systems, a crucial skill for managing global and multicenter trials.
GCP Recordkeeping and Source Documentation
A key focus of the Good Clinical Practice Certification is training professionals to implement ALCOA+ principles in all documentation: Attributable, Legible, Contemporaneous, Original, Accurate, Complete, and Enduring. This includes guidance on maintaining source documents, validating eCRF entries, managing protocol deviations, and ensuring audit trail traceability. Trainees review real-world scenarios where data integrity issues caused clinical holds, learning how to prevent these risks in daily operations. You also gain instruction on documenting informed consent processes, reconsent triggers, and version tracking aligned to regional IRB requirements.
FDA & EMA Readiness
Beyond GCP compliance, the certification actively prepares professionals for real audits. Learners are exposed to mock FDA inspections and interactive exercises that teach them how to defend TMF gaps, respond to 483 observations, and implement CAPA plans. CCRPS includes training on electronic system validation, ensuring you can assess whether your site's eTMF or eISF meets Part 11 requirements. The curriculum also covers EMA eTMF guidance, EU clinical trial regulation shifts, and how to document site-readiness for inspections across multiple authorities—especially for trials run across US/EU borders.
Designed for Working Professionals
Every module in the Good Clinical Practice Certification is self-paced and optimized for professionals already working in clinical settings. The platform integrates real SOP templates, TMF completeness checklists, and version-controlled ISF binder structures. You aren’t just learning what the rules are—you’re gaining plug-and-play frameworks that can be implemented on the job immediately. Whether you're a CRA, CRC, CTM, or regulatory affairs specialist, this certification helps close documentation gaps before they lead to protocol deviations or inspection findings.
Industry Recognition and Practical Impact
CCRPS has certified professionals across CROs, sponsor companies, and academic medical centers worldwide. The Good Clinical Practice Certification is fully accredited and recognized by global regulatory bodies and training alliances. Most importantly, it’s built by industry experts who’ve managed global documentation audits themselves. You’ll walk away with not only a credential but a complete toolkit to manage essential documents across all trial phases—from startup to closeout.
Frequently Asked Questions
-
ICH-GCP outlines a core list of essential documents required before, during, and after a clinical trial. These include the protocol and amendments, investigator’s brochure, informed consent forms, ethics committee approvals, and source documents. Sponsors must maintain a Trial Master File (TMF), while sites must keep an Investigator Site File (ISF). Key logs—like delegation of authority, screening, adverse event, and drug accountability—are also required. Proper version control, signatures, and archival standards must be followed. Failing to maintain these documents can result in delayed approvals or inspection findings that compromise data validity.
-
Retention periods vary by region and type of trial, but most GCP-compliant studies require document retention for at least 2 years after marketing approval or trial discontinuation. For example, the FDA mandates a 2-year minimum, while the EU Clinical Trial Regulation requires retention for 25 years in some cases. Sponsors must specify retention policies in agreements and ensure archival systems support long-term readability and access. Using validated eTMFs or secure physical storage is essential for meeting this obligation. Poor retention planning can lead to regulatory noncompliance or data loss during post-trial audits.
-
Source documents are the original records of trial-related observations and data—such as medical charts, lab reports, or patient diaries. Case Report Forms (CRFs), on the other hand, are structured tools used to collect and submit selected data points from the source. All CRF entries must be transcribed accurately from the source, with traceable corrections and audit trails. Regulatory authorities expect data integrity between both formats. Discrepancies—like mismatched dates, values, or investigator notes—can lead to serious findings under GCP audits. Maintaining alignment through ALCOA+ principles is essential for inspection readiness.
-
Yes, but only if systems meet FDA 21 CFR Part 11 and relevant EMA eTMF standards. Electronic records must be validated, secure, and include audit trails, e-signature controls, and access management. Sponsors and sites must also maintain SOPs covering digital workflows, metadata handling, and role-based permissions. However, replacing paper doesn’t remove the need for proper training—user errors remain a major audit risk, especially when electronic CRFs are modified without traceability. Regulators accept fully digital trials if documentation systems are proven compliant, accessible, and enduring over the retention period.
-
Among the most cited documentation issues during audits are: missing signatures, outdated SOPs, incomplete delegation logs, lack of version control, and misalignment between source documents and CRFs. Other frequent pitfalls include using outdated protocols, failing to document reconsent after amendments, or poor storage of electronic records. In global trials, issues like language inconsistencies or misfiled regulatory approvals can trigger country-specific findings. Auditors evaluate whether documents not only exist but also meet standards for timing, accuracy, and traceability. Even minor inconsistencies—like an unsigned visit note—can escalate to GCP violations.
-
Multicenter and global trials introduce complex variables like language localization, regional regulations, and document synchronization across time zones and platforms. For instance, some countries require IRB approvals at both institutional and national levels. Others enforce unique rules on consent formats, safety reporting, or data export. Central sponsors must ensure the TMF matches ISF records at every site, regardless of location. Without consistent versioning and cross-border training, document fragmentation becomes inevitable. In single-site trials, documentation is simpler to control, but still subject to full GCP standards and local IRB requirements.
-
The Good Clinical Practice Certification by CCRPS trains clinical professionals in the practical application of documentation standards across ISF, TMF, source records, and digital systems. It covers ALCOA+ principles, FDA and EMA audit protocols, protocol amendment tracking, and sponsor-site document reconciliation. Learners engage in real-world case studies, master electronic validation workflows, and receive tools like SOP templates and TMF checklists. The certification is fully accredited and ideal for CRAs, CRCs, CTMs, and regulatory professionals aiming to avoid audit findings and maintain inspection-readiness across global trials.
Final Thoughts
Clinical trial documentation isn’t just a regulatory obligation—it’s the structural integrity of trial success. From the first subject screened to the final regulatory submission, every log, form, and signature builds a defensible history of the study. Whether you're working in a single-site environment or managing a multicenter global trial, documentation errors aren’t tolerated—they’re penalized.
Professionals serious about advancing in this space must prioritize training that aligns with inspection standards. The Good Clinical Practice Certification delivers exactly that—equipping teams with the tools, systems, and protocols needed to maintain audit-ready documentation from day one. In an industry where compliance is constantly evolving, those who master documentation don’t just pass inspections—they drive clinical operations forward.
Quick Poll: What’s the biggest challenge you face with clinical trial documentation?